Complex Regional Pain Syndrome (CRPS) Treatment in Melbourne
Complex Regional Pain Syndrome (CRPS) is one of the most painful and misunderstood conditions we treat. It can develop after even a small injury, sprain, or surgery and the pain can be far worse than expected. Burning, stabbing, electric pain, skin sensitivity, colour changes, swelling, and stiffness are common.
The longer it is left undiagnosed and untreated, the more difficult it can be to manage.
At Pain Specialists Australia, our Melbourne-based team of expert pain specialists diagnose and treat CRPS early to reduce pain, restore function, and prevent long-term disability.
Key Takeaways
CRPS causes severe, disproportionate pain and sensitivity after an injury or surgery.
The trigger event can be minor in terms of severity but still cause severe CRPS
Early diagnosis and specialist treatment greatly are vital to improve recovery and function.
Pain Specialists Australia delivers multidisciplinary, evidence-based CRPS care across Melbourne by specialists in CRPS.
Treatment must be proactive and consider physiotherapy, occupational therapy, desensitisation, combination medications targeting nerve pain, nerve blocks, pulsed radiofrequency, infusions, or advanced therapies like neuromodulation.
When CRPS Takes Hold
CRPS warm phase with redness, swelling, warmth and marked skin sensitivity.
CRPS begins when the body’s nervous system overreacts to an injury. The pain persists long after the tissue has recovered and healed. Skin can feel like it is burning, freezing, or being crushed even from light touch, air, or clothing.
You may notice swelling, skin colour changes (pale, red, or purple), or unusual sweating in one limb. The affected area can feel cold or warm compared with the other side. Movement often becomes difficult, not because the joint is damaged, but because pain and sensitivity make you fearful to move.
Sometimes the limb doesn’t even feel like it’s part of your body anymore.
There are two main types:
CRPS Type I – develops after injury without confirmed nerve damage.
CRPS Type II – occurs when there is a documented nerve injury.
CRPS most often affects an arm, hand, leg, or foot and without treatment, it can spread to many other areas of your body.
Stages of CRPS from warm inflammatory phase to chronic cold phase with trophic changes.
VIDEO: The Devastating Pain of Complex Regional Pain Syndrome (CRPS): Causes and Mechanisms Explained
Understand the biology driving burning pain, allodynia, and colour or temperature changes in CRPS.
Why does a small injury lead to such severe pain? This short explainer covers the nerve, immune and blood-flow changes behind CRPS, and why touch or breeze can feel unbearable.
Dr Nick Christelis explains:
Peripheral and central sensitisation
Autonomic changes that alter colour and temperature
Why validation and early treatment matter
Understand Your Pain – Get Assessed Early
Early Diagnosis Matters
Many people with CRPS spend months searching for answers. Some are told it is in their head. Others are referred to specialists too late, after the condition has progressed. Early specialist assessment is vital, every day counts.
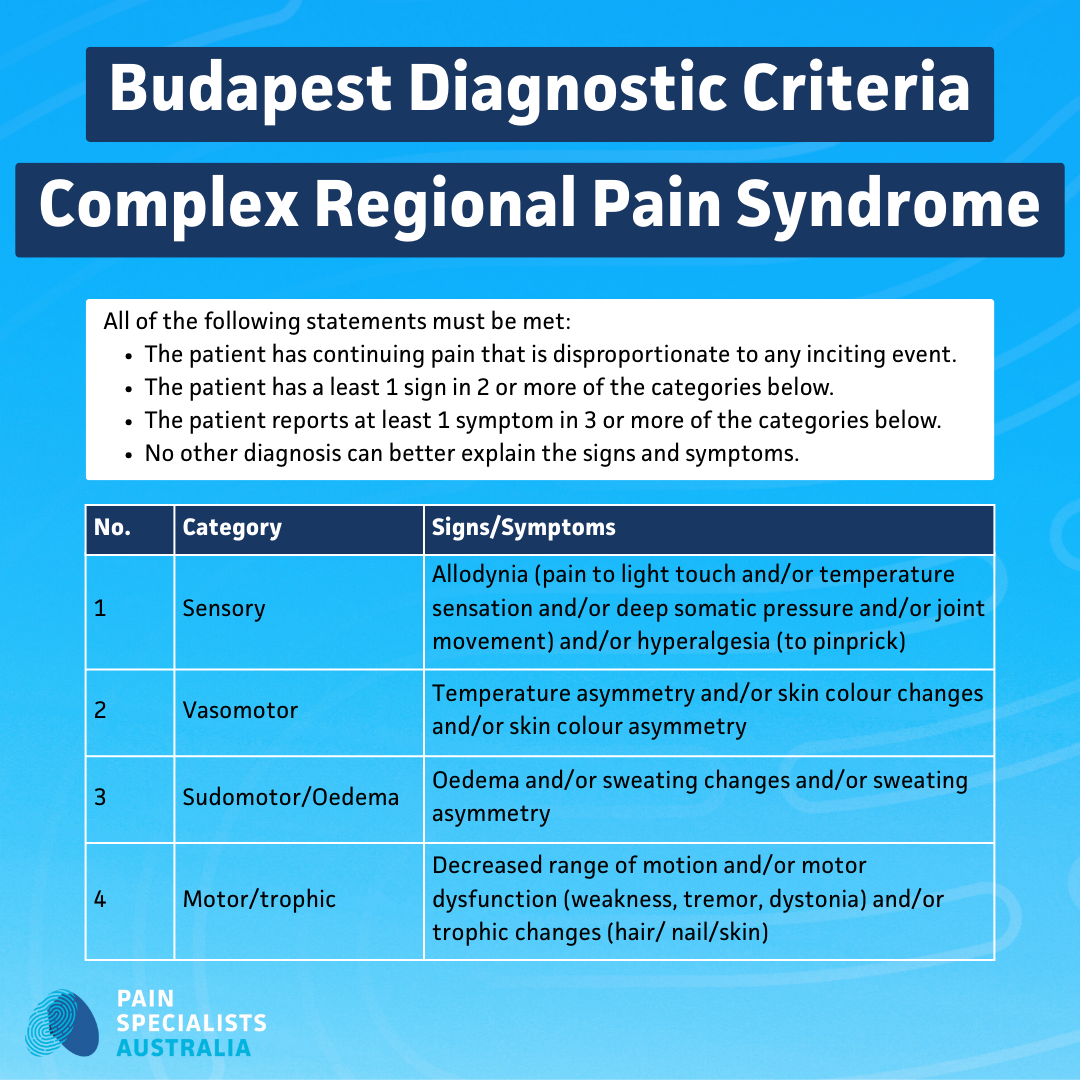
At Pain Specialists Australia, we use the internationally recognised Budapest Criteria to confirm CRPS. These include:
Pain that is disproportionate to the injury
Changes in skin temperature, colour, or sweating
Swelling and stiffness
Altered sensation (burning, electric, or painful to touch)
We combine clinical examination with selective imaging and nerve testing to exclude other causes. The goal is not just a label, but a clear, evidence-based plan that stops uncertainty and restores confidence.
Budapest Diagnostic Criteria used to confirm Complex Regional Pain Syndrome.
VIDEO: Where Can CRPS Develop? Doctors Answer Your Questions
Doctors explain upper and lower limb CRPS, why location matters for diagnosis, and the role of early specialist care.
CRPS can affect the hand, arm, foot or leg, and sometimes more than one area if untreated. In this Q&A we answer the common questions about where CRPS occurs and why it may feel like it spreads.
Our experts cover:
Upper vs lower limb patterns
Why pain can feel bigger than the injury
What to do if symptoms move or spread
Our Approach to CRPS Treatment
CRPS needs a coordinated, proactive stepwise plan. No single treatment works for everyone. Our approach combines medical, interventional, and rehabilitation therapies all delivered within one connected team.
VIDEO: Medications not helping your CRPS? You’re not alone. We discuss pain interventions and advanced pain management options for CRPS
Watch how specialist pain interventions in Melbourne are used when CRPS medications fall short, and how we decide who benefits.
If medication has not helped your CRPS, you are not stuck. In this video, our team explains advanced options such as image-guided nerve blocks, pulsed radiofrequency, ketamine or lignocaine infusions for selected cases, and neuromodulation.
Learn:
When to move beyond tablets
What a sympathetic block does and how it is guided
PRF, infusions, and when we consider them
Why procedures support rehab rather than replace it
Phase 1 - Reduce Sensitivity and Pain
Pain sensitivity in CRPS often stems from abnormal nerve signalling in both the limb and the spinal cord. We start by calming this system down.
Desensitisation therapy: Gradually retrains the skin and nerves to tolerate touch and movement.
Mirror therapy and graded motor imagery: Helps the brain reconnect safely with the affected limb.
Non-opioid medications: Such as gabapentinoids, certain antidepressants, anti-inflammatories, free-radical scavengers, all target pain nerve pathways. Sometimes even specialised creams can reduce skin sensitivity.
Stress and sleep regulation: Anxiety and poor rest can intensify symptoms; we do our best to stabilise both.
Phase 2 - Restore Movement and Function
Movement is vital for CRPS - but only when guided carefully.
Specialist physiotherapy: Gentle, progressive movement to reduce stiffness and fear of activity.
Occupational therapy: Rebuilds everyday skills and supports function and return to work or hobbies.
Psychological support: Addresses fear of pain, anxiety, and emotional exhaustion. Therapy such as CBT or ACT helps reframe and manage pain responses.
We focus on restoring confidence, not just reducing symptoms. You are never told to push through. We work at your pace with structured, measurable goals.
Phase 3 - Targeted Interventions (when needed)
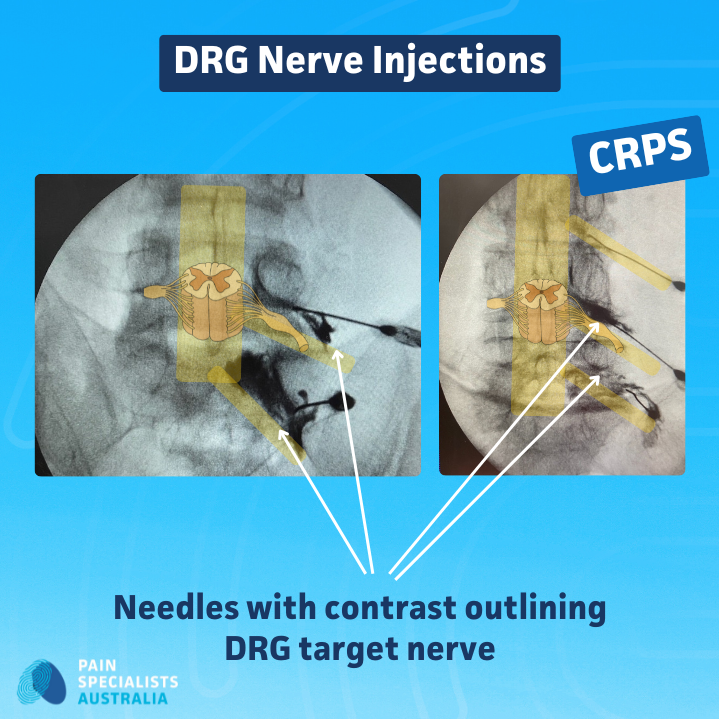
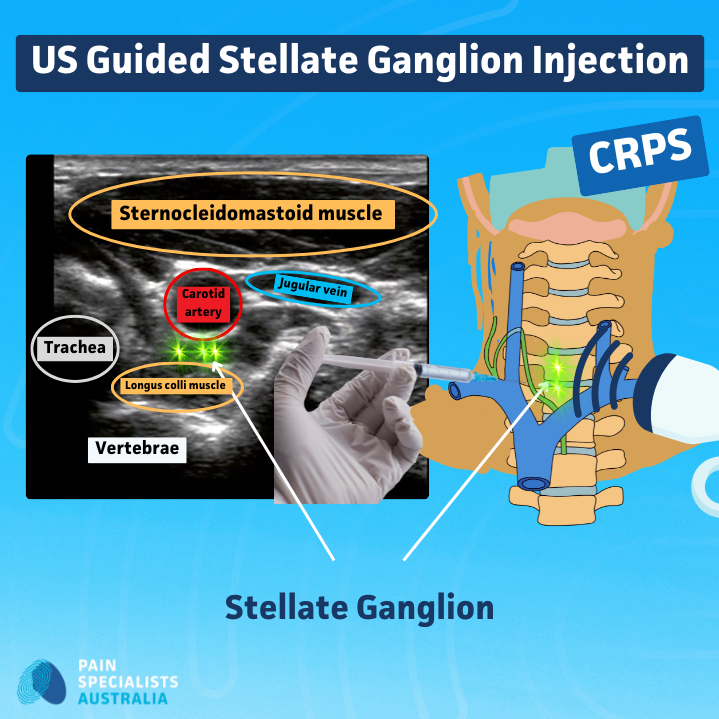
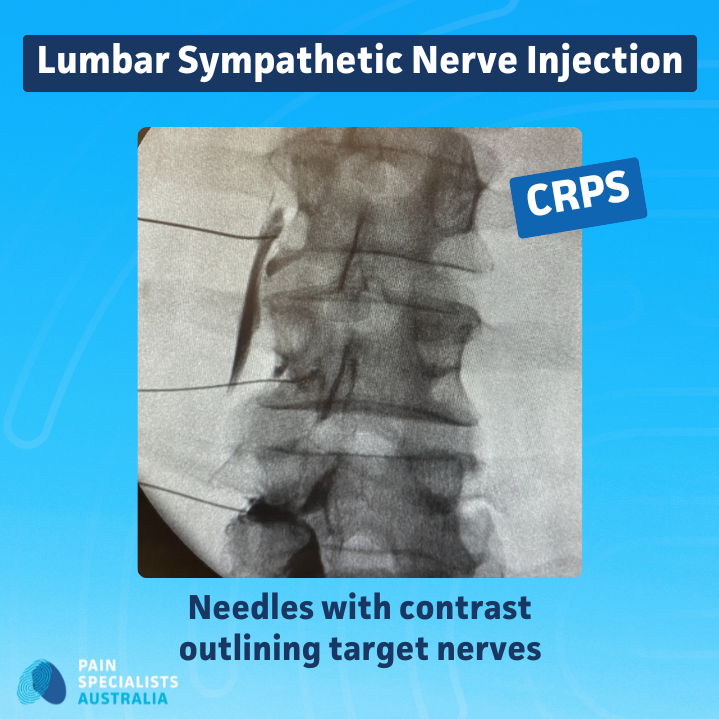
When pain remains severe despite rehabilitation, targeted procedures can calm overactive nerves and improve function.
Sympathetic nerve blocks
Image-guided injections that interrupt abnormal nerve signals driving CRPS pain. Relief can last weeks to months and may support ongoing rehabilitation.Pulsed Radiofrequency (PRF)
PRF uses low-intensity electrical energy delivered by needles, to modulate pain pathways without destroying nerves. It can provide longer relief than local anaesthetic blocks and can be safely repeated if needed.Neuromodulation (Spinal Cord or DRG Stimulation or intrathecal medication pumps)
In severe or refractory CRPS, small implanted devices can gently stimulate specific nerves or deliver micro-doses of medications to reduce pain signals where they occur. This is called targeted pain therapy. Neuromodulation is offered to carefully selected patients when other options have failed.IV infusion therapies
In some cases, controlled hospital-based infusions (for example lignocaine, ketamine) may help stabilise pain and reset nerve sensitivity.
Dorsal Root Ganglion (DRG) nerve injection with contrast outlining the target nerve.
Ultrasound-guided stellate ganglion injection targeting the sympathetic chain.
Fluoroscopy-guided lumbar sympathetic nerve injection showing contrast around target nerves.
Life After CRPS - Rehabilitation and Hope
Recovery from CRPS is a journey, not an event. It is common to feel frustrated, isolated, or fearful at first. Our role is to rebuild movement, confidence, and trust in your body.
We teach pacing and flare management strategies, so you can stay active without overdoing it. Gentle exercise, hydrotherapy, relaxation, and mindfulness help calm the overactive nervous system.
Flare-ups will happen, but with the right therapy tools and support, they no longer control your life.
VIDEO: 5 CRPS Myths Exposed - The Pain Diaries Podcast
We tackle five CRPS myths and give simple, evidence-based actions you can take to move forward.
A lot of online advice about CRPS is misleading. In this podcast segment we break down five common myths that delay recovery and increase fear, and replace them with practical steps that help.
Myth: Rest is best. Reality: guided, gentle movement helps.
Myth: Nothing can help. Reality: a stepwise plan often does.
Myth: Pain equals damage and harm. Reality: sensitivity can be trained down.
Myth: Stronger drugs are the only answer. Reality: an experienced pain specialist will have many possible treatment options.
Myth: You must do it alone. Reality: this is not true. Find your caring team.
Why Choose Pain Specialists Australia
Many people with CRPS feel unseen, unheard, or misdiagnosed. They can wait many months and even years to get into a pain clinic and when they are finally seen, they get given on therapy only. At Pain Specialists Australia, we take your pain seriously and we act quickly, we formulate a comprehensive plan of action.
Decades of clinical experience diagnosing and treating CRPS.
Expertise in interventional and multidisciplinary CRPS management.
Rapid private access (appointments often within days to a few weeks). We see 80% of referrals within 30 days of referral and we prioritise CRPS.
Integrated care with physiotherapy, psychology, and dietetics and other specialists.
Collaboration with your GP, surgeon, or neurologist.
Multiple clinic locations across Melbourne (Richmond, Heidelberg, and Bayside).
Fast access when it matters most
We prioritise CRPS and aim to see patients with acute and early-stage CRPS within days of referral. Once a referral is received, our team of nurses and administrative staff contact patients within 24 hours to arrange urgent assessment at the most convenient Melbourne location.We do not just prescribe; we diagnose, intervene, and restore.
What People Say About Living with CRPS
We listen closely to what people with CRPS share in clinics and online communities. Their stories help shape how we care for every new patient.
Here’s what we hear most often:
“It started after a small injury, but the pain never switched off.”
“Even clothes or a breeze can hurt — it’s impossible to explain to others.”
“It took months before someone recognised what was happening.”
“I just want to be believed and have a clear plan.”
“I’m scared it will spread. I need to know what to do next.”
These lived experiences remind us why early diagnosis and structured care matter so much. At Pain Specialists Australia, we work to replace fear with understanding and isolation with coordinated, expert support.
Frequently Asked Questions (FAQ)
1. What causes CRPS after a minor injury?
CRPS occurs when the body’s pain system becomes stuck in an overactive state. After an injury, instead of calming down, the nerves keep firing pain signals. They move into a fight or flight heightened state. Blood flow and immune responses also change, leading to swelling, colour shifts, and stiffness.
2. How is CRPS diagnosed in Australia?
Pain specialists use the Budapest Criteria, which assess pain, temperature, colour, swelling, and sensitivity. There is no single blood test or scan diagnosis relies on experience and careful examination. Scans and tests can help rule out other possible diagnoses like infection or vascular issues.
3. Can CRPS spread to other limbs?
Yes, but early treatment reduces that risk. The longer CRPS goes untreated, the higher the chance of spread or chronic sensitisation.
4. What treatments are available in Melbourne?
Pain Specialists Australia offers a full range: physiotherapy, desensitisation, graded motor imagery, nerve blocks, pulsed radiofrequency, infusions, and neuromodulation, all under one roof.
5. How long does CRPS take to improve?
It varies. If referred early and to the right team, many patients notice improvement within months once specialist care begins. For chronic cases, function and pain can continue improving over one to two years with consistent treatment.
6. What should I do during a flare?
Avoid total rest; gentle movement prevents stiffness. Use warmth, relaxation techniques, and desensitisation exercises. If a flare persists, contact your pain specialist for review.
References
Further Reading and References on CRPS:
1. Harden RN et al. Complex Regional Pain Syndrome: Practical Diagnostic and Treatment Guidelines, 5th Edition. Pain Med. 2022;23(Suppl 1):S1–S53.
- Latest multidisciplinary CRPS guidelines covering diagnosis, rehabilitation, pharmacological and interventional options, with emphasis on early functional restoration and coordinated care.
https://pubmed.ncbi.nlm.nih.gov/35687369/
2. Bruehl S. Complex regional pain syndrome. BMJ. 2015;351:h2730.
- State-of-the-art clinical review of CRPS, including epidemiology, mechanisms, diagnostic approach and evidence-based treatment strategies.
https://pubmed.ncbi.nlm.nih.gov/26224572/
3. Marinus J et al. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurol. 2011;10(7):637–48.
- Detailed overview of CRPS clinical presentation and underlying mechanisms, including peripheral and central sensitisation, autonomic changes and cortical reorganisation.
https://pubmed.ncbi.nlm.nih.gov/21683929/
4. Harden RN et al. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8(4):326–31.
- Seminal paper proposing the Budapest diagnostic criteria, addressing limitations of the original IASP criteria and improving diagnostic specificity for CRPS.
https://pubmed.ncbi.nlm.nih.gov/17610454/
5. Bean DJ, Johnson MH, Kydd RR. The outcome of complex regional pain syndrome type 1: a systematic review. J Pain. 2014;15(7):677–90.
- Systematic review of CRPS type 1 prognosis showing many patients improve within 6–13 months, but a substantial group has persistent pain and disability, with generally low-quality evidence.
https://pubmed.ncbi.nlm.nih.gov/24530407/
6. Johnson S et al. Complex regional pain syndrome what is the outcome? A systematic review. Eur J Pain. 2022;26(6):1203–1220.
- More recent systematic review demonstrating that pain and motor dysfunction frequently persist beyond 12 months, with significant impacts on grip strength, range of motion and participation.
https://pubmed.ncbi.nlm.nih.gov/35435302/
7. Cossins L et al. Treatment of complex regional pain syndrome in adults: a systematic review of randomized controlled trials published from June 2000 to February 2012. Eur J Pain. 2013;17(2):158–73.
- Critical review of CRPS RCTs showing a limited but growing evidence base, with some support for bisphosphonates, corticosteroids, calcitonin and graded motor imagery among other interventions.
https://pubmed.ncbi.nlm.nih.gov/23042687/
8. van Eijs F et al. Evidence-based interventional pain medicine according to clinical diagnoses. Complex regional pain syndrome. Pain Pract. 2011;11(1):70–87.
- Interventional pain review for CRPS summarising the evidence for sympathetic blocks, spinal cord stimulation and other procedures within a structured treatment algorithm.
https://pubmed.ncbi.nlm.nih.gov/20807353/
9. Connolly SB et al. A systematic review of ketamine for complex regional pain syndrome. Pain Med. 2015;16(5):943–69.
- Systematic review concluding that ketamine shows promise for refractory CRPS but current trials are small and of moderate to low quality, so evidence remains weak and further studies are needed.