Chronic Stomach (Abdominal) Pain - When It Won’t Go Away
Chronic stomach (abdominal pain) can be exhausting and debilitating.
Most people experience stomach pain at some point. Usually it settles on its own, or a GP, gastroenterologist or surgeon identifies a clear cause and treats it.
But what if the pain doesn’t go away? What if your abdominal pain becomes chronic and long lasting?
Some people continue to have pain for months or even years after surgery or treatment, despite normal tests and scans. The pain may come from deep inside the abdomen or from nerves in the abdominal wall.
Important: If your pain is sudden, severe, or keeps getting worse, or if you have symptoms such as vomiting blood, black or bloody stools, fever with severe pain, chest pain, yellow skin or eyes, difficulty passing urine or gas, or you are pregnant and in pain, call 000 or go to the emergency department now.
Our role at Pain Specialists Australia is to help when abdominal pain becomes chronic and complex, not when urgent care is needed.
First consult focused on fast diagnosis and clear next steps.
Symptoms of Chronic Abdominal Pain
People with chronic abdominal pain often describe:
Burning, stabbing, gnawing, or “tight band” sensations.
Pain that gets worse when tensing the stomach muscles.
Ongoing pain after surgery, such as gallbladder removal, hernia repair, laparoscopy, laparotomy or any other abdominal surgery.
Upper abdominal pain that radiates through to the back, common in chronic pancreatitis.
Fear of eating, disrupted sleep, fatigue, and loss of confidence in everyday life.
Causes of Persistent Stomach Pain
Carnett’s sign helps identify whether abdominal pain arises from the abdominal wall or deeper organs.
Post-surgical pain syndromes
Chronic pain can follow procedures such as gallbladder removal (post-cholecystectomy), hernia repair, bowel surgery, C-section, or laparotomy/laparoscopy. Nerve injury, scar tissue, or mesh-related irritation are common causes.
Abdominal wall nerve entrapment (ACNES)
This is one of the most under-recognised causes of long-term abdominal pain. Abdominal Cutaneous Nerve Entrapment Syndrome (ACNES) typically causes sharp, burning pain in a finger-sized spot that is tender to press and worse when tightening the abdominal wall. It is often misdiagnosed and not even understood by many health professionals. A bedside test called Carnett’s sign helps confirm this diagnosis.
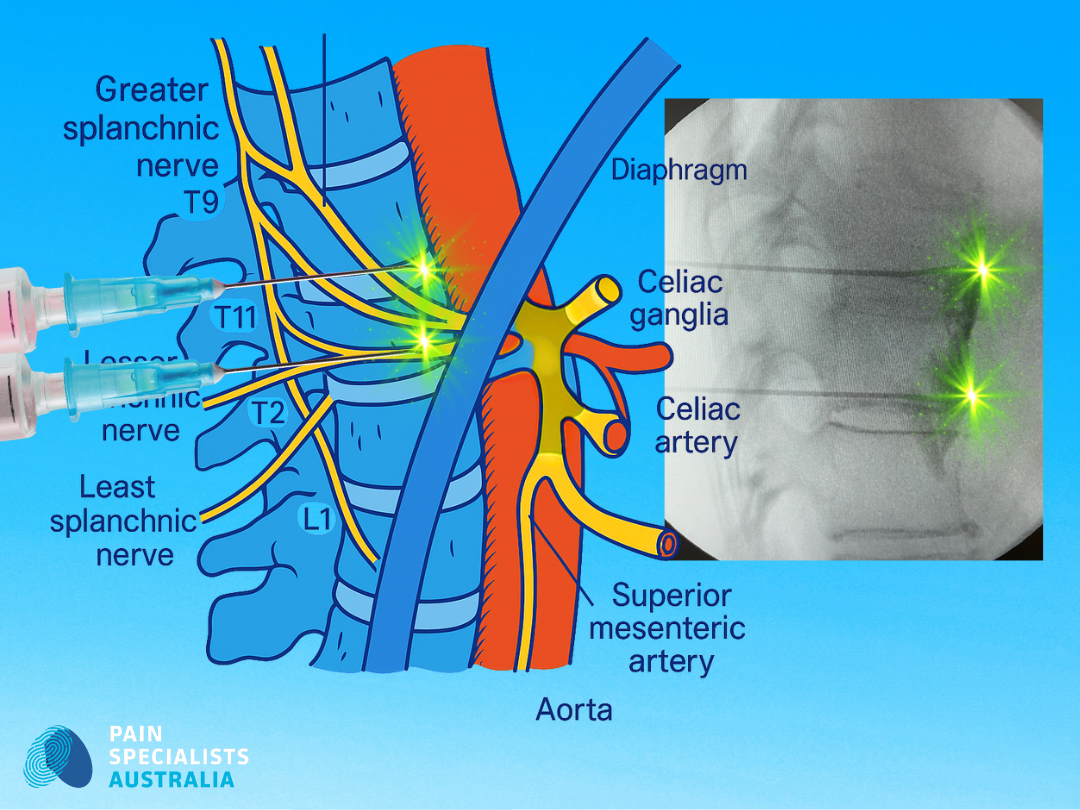
Image-guided splanchnic plexus block for selected upper abdominal pain.
Chronic pancreatitis and upper abdominal syndromes
Chronic pancreatitis can cause relentless epigastric pain that radiates into the back, worsens after meals, and can lead to food fear and weight loss. In selected cases, treatments might include image-guided coeliac plexus or splanchnic nerve blocks, sometimes followed by radiofrequency, can reduce pain and improve quality of life.
Nerve pain (neuropathic pain) and central sensitisation pain
Sometimes all the tests come back normal, but the pain is still real. This can occur when nerves in the abdominal wall are overactive, or when the nervous system itself becomes sensitised. This explains why pain persists even when scans look “normal.”
This is often overlooked as a cause of chronic abdominal pain.
What is visceral hypersensitivity?
Visceral hypersensitivity means the nerves of the gut become overly sensitive, so normal signals from the stomach or intestines are felt as pain. It is thought to play a major role in conditions like irritable bowel syndrome and functional abdominal pain. Treatments may include gut-directed therapies, medications that calm nerve activity, and psychological strategies to retrain how the brain interprets pain signals.
What is opioid-induced hyperalgesia?
Opioid-induced hyperalgesia happens when long-term use of opioid medicines actually makes the nervous system more sensitive to pain instead of less. This can show up as worsening stomach or body pain despite increasing doses of opioids. Reducing or stopping opioids under specialist guidance, and switching to targeted non-opioid treatments, can help reset pain sensitivity.
Why Choose Pain Specialists Australia?
We have decades of combined experience and subspecialist expertise in chronic abdominal pain syndromes like chronic abdominal wall, post-surgical, and chronic pancreatitis pain.
Precision image-guided procedures for safe, targeted treatment.
Multidisciplinary team including pain specialists, physiotherapists, psychologists, and dietitians.
Pain is complex. That’s why we don’t treat it simply.We recognise that chronic pain involves nerves, emotions, sleep, movement, and life impact and we treat all of it.
A commitment to realistic goals: improving sleep, movement, and quality of life.
No patient leaves wondering what comes next. Clarity reduces fear. Every consult ends with a documented, explained plan.
What People Say About This Pain
Hearing the words of patients makes clear just how much chronic stomach pain affects daily life:
“Every test is normal. I’m still in unbearable pain.”
“Phantom gallbladder pain… nothing on scans. They say it’s nerve pain.”
“Burning groin pain after hernia repair - it never went away.”
Impact themes that affect patients include:
Fear that the pain is cancer or something serious.
Frustration at being told it is “just stress” or “IBS.”
Fear of food and disrupted sleep.
Missing work, cancelling social plans, and feeling dismissed.
At PSA, our first step is listening, validating the pain, exploring the history, and identifying patterns that may have been overlooked & setting up a treatment plan of action.
How We Diagnose Chronic Stomach Pain
Specialist assessment & examination
We start by listening and taking a careful story and perform a focused examination, including abdominal wall and spine assessment. Carnett’s sign is used to help distinguish organ-based pain from abdominal wall pain.
Diagnostic nerve blocks
In selected cases, a small local anaesthetic injection can pinpoint whether pain is arising from a specific nerve or plexus. If the injection helps, it confirms the diagnosis and guides treatment and next steps.
Smarter use of imaging and tests
We coordinate bloods, ultrasound, CT, MRI or endoscopy only if needed, usually through your GP or gastroenterologist. We aim to avoid unnecessary or repeat testing.
Targeted Treatments for Ongoing Abdominal Pain
Nerve and TAP blocks
Image-guided Transversus Abdominis Plane (TAP) blocks or trigger-point injections can help diagnose and also relieve abdominal wall and post-surgical nerve pain.
Radiofrequency ablation
If nerve blocks provide short-term benefit, radiofrequency (thermal or pulsed) can extend relief by reducing nerve over-activity. This needs to be performed by experienced and trained pain specialists such as our pain specialists at Pain Specialists Australia.
Coeliac & splanchnic plexus blocks
For selected people with chronic pancreatitis or more complex or widespread upper abdominal pain, these procedures target the sympathetic nerves that carry pain signals from the organs. These are specialised treatments that should be performed by experienced and trained pain specialists such as our pain specialists at Pain Specialists Australia.
Advanced neuromodulation
For severe, long-standing neuropathic abdominal pain that has not improved with other therapies, neuromodulation techniques can reduce pain intensity, support better sleep, and lower medication use. These are specialised treatments that should be performed by experienced and trained pain specialists such as our pain specialists at Pain Specialists Australia.
Rehabilitation and support
We pair treatments with physiotherapy, psychology-informed approaches, and dietitian support to reduce flare-ups and restore confidence.
Abdominal wall nerves can be a hidden source of ongoing abdominal pain.
Frequently Asked Questions (FAQ)
1. How do I know if my stomach pain is serious?
Seek urgent care if you have chest pain, black or bloody stools, persistent vomiting, fever with severe pain, or sudden tearing pain. These may signal a medical emergency. For ongoing or recurrent pain, a pain specialist can assess the source, explain why it is happening, and guide the right treatment plan.
2. Why do I still have pain after gallbladder or hernia surgery?
Some people continue to have pain for months or years after surgery, even if their scans look normal. Pain may come from trapped nerves in the abdominal wall, irritation of scar tissue, or deeper structures that do not always show up on imaging.
You don’t have to suffer with this pain. A specialist assessment helps separate surgical complications from nerve-related pain.
3. What if my scans are normal but I still hurt?
Not all causes of stomach pain show up on scans. Nerve entrapment, abdominal wall pain, or myofascial trigger points can be missed by imaging. Careful examination with tests like Carnett’s sign, combined with diagnostic nerve blocks, can help confirm the diagnosis and direct treatment.
4. What is abdominal wall nerve entrapment (ACNES)?
Abdominal Cutaneous Nerve Entrapment Syndrome (ACNES) occurs when small nerves in the abdominal wall get trapped, leading to sharp or burning pain. It can be confused with internal organ pain, but the difference is often clear on examination. Relief after a small local anaesthetic injection helps confirm the diagnosis and guide longer-term treatment options.
5. What is Carnett’s sign?
Carnett’s sign is a simple bedside test used by specialists to separate abdominal wall pain from internal organ pain. You tense your abdominal muscles while the doctor presses the sore spot, and if the pain gets worse, it usually means the problem is in the wall, not the organs. This test is quick, safe, and often very revealing.
6. What is a TAP block and when is it used?
A Transversus Abdominis Plane (TAP) block is an injection that numbs the nerves of the abdominal wall. It is commonly used after abdominal surgery to reduce pain and in some patients with chronic abdominal wall pain. A TAP block can lower pain levels, reduce opioid use, and for some people, may prevent ongoing postsurgical pain.
7. What is a splanchnic plexus block?
A splanchnic plexus block targets the sympathetic nerves that carry pain from the upper abdominal organs. The procedure is performed with X-ray or CT guidance to safely deliver local anaesthetic, steroids, or radiofrequency energy to those nerves. It is often considered when conditions such as chronic pancreatitis cause pain that has not responded to other treatments.
8. Can chronic pancreatitis pain be treated without opioids?
Yes, there are options for managing chronic pancreatitis pain without relying on opioids. Treatments may include nerve blocks, radiofrequency ablation, diet changes, and specialist rehabilitation to improve quality of life. Opioids are sometimes used, but they are rarely the best long-term solution and can often be avoided.
9. How long do nerve blocks or radiofrequency last?
The relief from a nerve block or radiofrequency procedure can vary. The aim is for pain reduction that lasts for many months and even years of improvement. Results may vary but with careful assessment, planning and execution the therapy can provide meaningful relief. If pain comes back, the procedure can often be repeated, and specialists may adjust the technique to provide more durable relief.
10. Who should I see for ongoing stomach pain in Melbourne?
If you have ongoing stomach pain that persists after surgery, or if scans have been normal, it is worth seeing a pain medicine specialist. They can work out whether pain is coming from the gut, the abdominal wall nerves, or another source. Your GP can organise a referral so you can access a personalised treatment plan designed around your needs.
11. Do I need a referral and is Medicare available?
Yes, you will need a referral from a GP or specialist to see a pain medicine specialist and to claim a Medicare rebate. After your consultation, we will send a detailed letter back to your GP with our findings and the treatment plan. This ensures your care stays connected and coordinated.
12. Will my gastroenterologist still be involved?
Yes, we work alongside your gastroenterologist rather than replacing them. Our role is to identify and treat pain drivers such as nerve-related or abdominal wall pain, which may not be within your gastroenterologist’s scope. This collaborative approach makes sure all aspects of your stomach pain are addressed.
Next Steps - Take Back Control
You don’t have to live with ongoing abdominal pain without answers.
Our specialists in Melbourne offer targeted diagnosis and evidence-based treatments to help you move forward.
References
Further Reading and References on Stomach Pain Management:
1. Ford AC, et al. Chronic Visceral Pain: New Peripheral Mechanistic Insights and Resulting Treatments. Gastroenterology. 2024 Jun;166(6):976-994.
- How advances in understanding peripheral nerve and gut–brain mechanisms of chronic visceral pain are leading to new, more targeted treatment strategies beyond traditional symptom control.
https://pubmed.ncbi.nlm.nih.gov/38325759/
2. Coffin B, Duboc H. Review article: diagnostic and therapeutic approach to persistent abdominal pain beyond irritable bowel syndrome. Aliment Pharmacol Ther. 2022 Aug;56(3):419-435.
- How persistent abdominal pain that is not explained by irritable bowel syndrome requires a structured diagnostic approach and may benefit from targeted therapies including neuromodulation, psychological strategies, and specialised pain interventions.
https://pubmed.ncbi.nlm.nih.gov/35656644/
3. Sweetser S. Abdominal Wall Pain: A Common Clinical Problem. Mayo Clin Proc. 2019.
- High prevalence; many “functional” cases are actually abdominal wall pain; outlines practical diagnosis/management.
https://pubmed.ncbi.nlm.nih.gov/30711130/
4. Koop H, et al. Chronic Abdominal Wall Pain. Dtsch Arztebl Int. 2016.
- Reviews ACNES and abdominal wall pain; emphasises Carnett’s sign and injections as diagnosis/treatment.
https://pubmed.ncbi.nlm.nih.gov/26883414/
5. Alnahhas MF, et al. Outcomes of Ultrasound-Guided Trigger Point Injection for Abdominal Wall Pain. Dig Dis Sci. 2016.
- Demonstrates effectiveness of ultrasound-guided trigger injections for abdominal wall pain.
https://pubmed.ncbi.nlm.nih.gov/26320087/
6. Pan Z-Y, et al. TAP block & chronic pain after colorectal surgery (retrospective cohort). BMC Anesthesiol. 2020.
- TAP block associated with less chronic postsurgical pain at 3–6 months after colorectal surgery.
https://pubmed.ncbi.nlm.nih.gov/32423381/
7. Lissauer J, et al. Evolution of the TAP block & role in postoperative analgesia. Best Pract Res Clin Anaesthesiol. 2014.
- Authoritative review on TAP block techniques, safety and indications.
https://pubmed.ncbi.nlm.nih.gov/24993433/
8. Kapural L, et al. Percutaneous Radiofrequency Ablation of the Splanchnic Nerves in Chronic Pancreatitis. Pain Med. 2013.
- Early evidence supporting splanchnic RFA for refractory visceral abdominal pain.
https://pubmed.ncbi.nlm.nih.gov/23301539/
9. Garcea G, et al. Percutaneous splanchnic nerve radiofrequency ablation for chronic abdominal pain. ANZ J Surg. 2005 Aug;75(8):640-4.
- In 10 chronic pancreatitis patients, percutaneous splanchnic RFA improved pain and quality of life, reduced opioid use/admissions, and had no major complications; larger comparative trials are needed.
https://pubmed.ncbi.nlm.nih.gov/16076323/
10. Shian B, Larson ST. Abdominal Wall Pain: Clinical Evaluation & Treatment. Am Fam Physician. 2018.
- Practical summary: use Carnett’s sign; consider diagnostic/therapeutic injections.