Facet Joint Pain Treatment
Facet joint pain is a common, often-missed cause of back or neck pain that worsens with extension or twisting, best confirmed with medial branch blocks and treated with targeted injections and radiofrequency ablation at Pain Specialists Australia in Melbourne.
Also called: facet arthropathy, facet syndrome, zygapophysial joint pain.
The facet joints run up and down the entire spine so could cause lower back pain or neck pain or even thoracic pain.
Typical pattern: deep axial ache with possible referral to buttock, hip, groin, or back of head.
Why it is missed: MRI or scans can be normal or not match symptoms.
The Pain Specialists Australia (PSA) approach: diagnosis-first with targeted medial branch blocks, then a matched treatment plan including medication, physiotherapy and, when indicated, radiofrequency ablation.
These evidence-based therapies relieve pain, restore movement, and help people walk and stand longer, sleep better, and reduce medication so you can get back to living your life.
Key Takeaways
The best treatment for facet joint pain is radiofrequency ablation done by experts like pain specialists. But you’ve got to get the diagnosis first.
Facet joint pain usually feels like a deep ache that is worse with extension and rotation and often eases when sitting or leaning forward. It can refer to the buttock, hip, groin, or the back of the head, but it is not classic sciatica.
Scans can be normal or show arthritis that does not match symptoms. Diagnosis is best confirmed with image-guided medial branch blocks, not imaging alone.
Start with a diagnosis-first then set up a treatment plan: targeted physiotherapy, activity pacing, and short courses of non-opioid medicines for flares while confidence and movement are rebuilt.
If medial branch blocks provide clear, reproducible relief, radiofrequency ablation (neurotomy) can switch off the tiny facet nerves for longer benefit. Relief typically lasts months and can be repeated if pain returns.
Sharp leg pain with pins and needles, numbness, or weakness suggests nerve root pain rather than facet joints and needs separate assessment.
Red flag (danger) symptoms that need urgent medical review include weakness, fever, unexplained weight loss, night pain, recent trauma, cancer history, or new bladder or bowel symptoms.
In Melbourne, care is usually coordinated by a pain specialist physician working with physiotherapy and psychology to support long-term recovery.
Facet joints are the small stabilising joints at the back of the spine.
What Is Facet Joint Pain?
Facet joints are small stabilising joints at the back of the spine that can become inflamed or arthritic and cause a deep, movement-linked ache.
Names and anatomy: zygapophysial joints, the “little hinges” guiding spinal motion.
Why they hurt: age-related change, degeneration, repetitive load, injury, prolonged extension or rotation.
Regions: lumbar (low back), thoracic (chest), cervical (neck).
Clinical importance: a very common, under-recognised source of chronic axial spine pain even with normal scans.
Facet joint pain can cause local back ache and referred pain to the buttock or hip.
Common Symptoms of Facet Joint Pain
Expect a deep local ache that flares with standing still, arching back, or twisting, and may refer to nearby areas rather than shoot down the leg like true sciatica or nerve pain.
Localisation: midline or paramedian back or neck ache.
Provocation: extension, rotation, prolonged standing.
Time pattern: morning stiffness or stiffness after activity.
Referral pattern: buttock, hip, groin, upper thigh, or back of head.
These patterns can help your pain specialist distinguish facet-mediated back pain from disc problems, nerve compression or other causes of back pain. A proper assessment and diagnosis by an experienced pain specialist is usually needed.
When It Is Probably Not Facet Joint Pain
Not all back or neck pain comes from the facet joints. Other conditions can cause similar symptoms, and it is important to recognise when the pattern does not fit. Sometimes it takes a pain management expert to help you make the differentiation
True sciatica or nerve compression: If pain shoots sharply down the leg, often with tingling, numbness, or weakness, the cause is more likely a disc pressing on a nerve root rather than the facet joints.
Sacroiliac joint pain: Pain that sits very low in the back or pelvis, often worse when standing from a chair or climbing stairs, may come from the sacroiliac joints rather than the spine itself.
Widespread pain syndromes: Conditions like fibromyalgia can cause widespread aching and fatigue, rather than the localised stiffness and movement-related pain typical of facet joint pain.
Red flags: Severe or sudden pain with weight loss, fever, bladder or bowel changes, or recent trauma should be assessed urgently as these can indicate other causes that need different management.
Why this matters: Facet joint pain has a distinct pattern of stiffness, deep aching, and worsening with extension or standing. If your pain does not follow this pattern, a specialist assessment should help rule out other causes and guide you to the right diagnosis and treatment.
How Facet Joint Pain Is Diagnosed
Many people ask if an MRI or X-ray can show facet joint pain. The answer is not always. Scans may reveal arthritis or age-related changes in the facet joints, but this does not always explain symptoms. Some people have severe arthritis on imaging with no pain, while others experience significant pain despite normal scans.
A careful physical examination by a pain specialist can provide important clues. Pressing over the facet joints or moving the spine into certain positions, such as arching backwards or twisting, may reproduce the pain. This can suggest the joints are involved, but it is not enough for certainty.
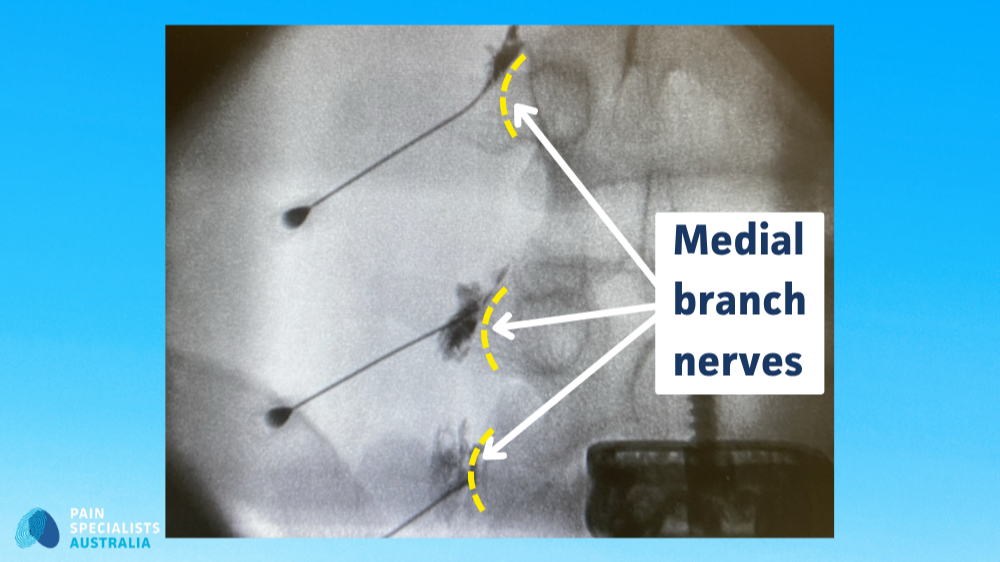
At Pain Specialists Australia, our experts confirm the diagnosis with a diagnostic medial branch block. Using live X-ray guidance, a small amount of anaesthetic is placed on the tiny nerves that supply the facet joints. If pain eases, it proves the joints are the true source and helps guide the next step in treatment.
In selected cases, advanced imaging such as SPECT scans may also help identify which joints are active pain generators.
Lumbar medial branch blocks (facet joint injections) help confirm facet joint pain and guide further treatment.
What Patients Tell Us
People with facet joint pain often describe a pattern that feels both frustrating and exhausting.
Many talk about a deep, aching stiffness in the back or neck, often worse in the morning or after long periods of standing. Others notice that the pain flares when they arch backwards or twist, but eases when they sit down or lean forward.
It is also common to describe the pain as spreading into the buttock, hip, groin, or even the back of the head, which can make it hard to tell apart from other spinal problems. Some say the experience feels like an invisible burden, affecting their ability to walk, work, sleep, or simply get through the day without flare-ups.
A frequent theme is uncertainty. Many people feel stuck when scans look normal, or when earlier treatments give only short-lived relief. What they want most is clarity about where the pain is really coming from and a clear plan for managing it.
The most helpful shift is a clear diagnosis with a structured plan and measurable progress.
Treatment Options for Facet Joint Pain
Start conservative treatment with targeted physiotherapy and flare control with medication, then confirm the diagnosis with medial branch blocks, then use radiofrequency ablation for longer relief when blocks are positive.
Physiotherapy and Lifestyle Support
Targeted physiotherapy is often the first step in managing facet joint pain. Physio reduces joint load and improves control, so the spine tolerates movement without flares.
Focus: endurance and motor control of deep stabilisers, posture retraining, graded exposure.
Tools: activity pacing, movement hygiene, flare plans.
Benefits: less morning stiffness, better walking and standing tolerance, confidence to move.
Medications and Short-Term Injections
Short courses of non-opioid medicines and occasional facet steroid injections can settle flares while the long-term plan takes effect.
Medicines: anti-inflammatories, short courses of muscle relaxants or neuropathic agents as needed.
Facet steroid: targeted peri-articular or intra-articular injection for short-term relief.
Role: bridge therapy alongside physio and diagnostic blocks, not a stand-alone solution.
Medial Branch Blocks (Diagnostic and Therapeutic)
A medial branch block is a low-volume local anaesthetic at the medial branches confirms the facet as the pain source and predicts radiofrequency success.
Purpose: diagnostic first, short-term therapeutic benefit is a bonus.
Setting: specialist procedural suite using live imaging.
Next step: proceed to radiofrequency ablation if relief is clear and reproducible.
At Pain Specialists Australia, these blocks are part of a complete diagnostic and treatment pathway that includes physiotherapy, radiofrequency treatment, and longer-term support rather than one-off procedures.
Radiofrequency Ablation (Neurotomy) for Longer Relief
When a medial branch block confirms that the facet joints are the true source of pain, the next step is a radiofrequency ablation switches off facet nerve signals and commonly gives months of improved function with repeatable results.
Method: precise needle placement under X-ray, controlled heat lesions at medial branches.
Duration: often 6 to 18 months, repeatable when pain returns.
Outcomes: longer walking and standing tolerance, better sleep, less medication.
Pain Specialists Australia setting: accredited private hospitals across Melbourne, including Windsor, Heidelberg, and Bayside.
Radiofrequency treatment can provide longer-term relief from facet joint pain.
Radiofrequency treatment uses precise needle placement to target the facet joint nerves.
Restorative Multifidus Muscle Stimulation
For persistent mechanical low back pain with multifidus dysfunction, restorative neurostimulation re-activates the deep stabiliser to address a root cause rather than only the symptom.
Rationale: impaired multifidus control increases facet loading and flare risk.
Suitability: documented multifidus dysfunction after conservative and interventional care.
Goal: rebuild spinal stability, reduce flare frequency, improve long-term function.
Why Choose Pain Specialists Australia?
We are a college accredited pain clinic with FFPMANZCA pain specialists that deliver diagnosis-first care, evidence-based procedures, and integrated rehabilitation across Melbourne.
Quality: medial branch blocks and radiofrequency under live imaging in accredited Richmond, Heidelberg, and Bayside hospitals.
Multidisciplinary: physicians, physiotherapists, psychologists, and dietitians working to your goals
Volume and access: we assess and treat thousands of chronic spine patients each year across our PSA clinics.
There’s always a reason. We help you find it.
Frequently Asked Questions (FAQ)
1. What makes facet pain worse and what makes it better?
Extension and rotation usually aggravate it, and gentle movement plus flexion-bias postures often help.
Worse: standing still, arching back, twisting
Better: sitting, leaning forward, regular gentle movement
2. Can facet joints cause sciatica-like pain?
They can refer to the buttock, hip, groin, or thigh, but true sciatica is a nerve-root problem with dermatomal shooting pain and possible numbness or weakness.
Understanding this distinction is important because treatments for facet pain and sciatica are very different.
3. Will physiotherapy help or make it worse?
Physio helps when it targets control and endurance with flare-aware progression.
Focus: deep stabilisers, posture, graded exposure
Outcome: fewer flares and safer movement
4. Do X-rays or MRI confirm facet joint pain?
Not reliably. Imaging is supportive, but medial branch blocks confirm the diagnosis.
5. How is facet pain diagnosed if scans are normal?
With image-guided medial branch blocks that temporarily numb the suspected joints.
6. What is a medial branch block and why is it diagnostic?
A medial branch block is a small injection placed under X-ray guidance on the nerves that carry pain signals from the facet joints.
If pain improves for the duration of the anaesthetic, it shows that the facet joints are the likely cause.
This test guides whether longer-lasting treatments such as radiofrequency ablation may help. It is an essential step before moving on to more durable procedures.
7. Facet injection vs medial branch block vs radiofrequency – what is the difference?
A facet injection places steroid into or near the joint for short-term relief.
A medial branch block numbs the tiny nerves supplying the joint and is mainly used to confirm diagnosis.
Radiofrequency ablation (RFA) uses controlled heat to switch off those nerves for longer-lasting relief, often many months and sometimes even years.
Each has a different purpose, and specialists usually use them in sequence as part of a structured treatment pathway.
8. How long do results last and can it be repeated?
Relief from a medial branch block usually lasts only hours or days. Sometimes longer.
If radiofrequency ablation is successful, pain relief often lasts 6–18 months and the procedure can be safely repeated if pain returns.
This stepwise approach helps people manage pain over the long term while avoiding unnecessary surgery.
9. Who should do facet joint injections — a radiologist or a pain specialist?
Both radiologists and pain specialists can perform procedures such as facet joint injections and medial branch blocks, but pain specialists integrate diagnosis, procedures, and long-term care.
Radiologists can do the procedures. They are experts in medical imaging and use X-ray, CT, or ultrasound to place the needle accurately. Their focus is on the scan and the technical procedure itself. In most radiology clinics, the injection is done as a single service and the radiologist may not take a full pain history, examination or provide ongoing care.
Pain specialists can expertly perform these procedures, but they also bring together the whole picture. They start with a detailed history and physical examination, review your scans, and decide if the facet joints are likely to be the pain source. If injections confirm this, they plan the next steps, which may include radiofrequency ablation, physiotherapy, or longer-term strategies.
In short, radiologists follow the scans, while pain specialists follow the history, examination, and scan findings together. This means injections done under a pain specialist are not just technically accurate, but also part of a comprehensive treatment pathway aimed at reducing pain, improving mobility, and restoring quality of life.
10. What are the risks of injections and radiofrequency?
Both facet joint injections and radiofrequency ablation are considered low risk when performed under X-ray guidance by trained specialists.
Possible side effects include:
Temporary soreness at the injection site, mild bruising, or short-lived numbness in the back or neck.
Some people may feel an increase in discomfort for a day or two before the pain improves.
Serious complications are very rare and might include infection, bleeding, nerve injury.
Most people are able to return to normal activities within a day or two, making these safe options for many with chronic back or neck pain. Your pain specialist will discuss the risks, benefits, and alternatives in detail before the procedure. This gives you the chance to have all your questions answered and ensures you feel fully informed before deciding on treatment.
11. Do I need a referral and is Medicare available?
Yes, you will need a referral from a GP or specialist to see a pain specialist. In Australia, Medicare rebates apply to medial branch blocks and radiofrequency ablation when performed by qualified specialists in accredited facilities. This means patients in Melbourne can access these treatments as part of standard medical care.
Book Facet Joint Pain Treatment in Melbourne
If you are living with ongoing back or neck pain that gets worse when standing, arching backwards, or twisting, the problem may be coming from your facet joints.
A proper diagnosis is the key to moving forward.
Speak with your GP about a referral to Pain Specialists Australia.
Our team uses advanced diagnostics such as medial branch blocks and evidence-based treatments including facet joint injections and radiofrequency ablation.
With clinics across Melbourne, we help people find answers, reduce flare-ups, and return to moving, sleeping, and living with greater ease.
References
Further Reading and References on Facet Joint Pain:
1. Kalichman L, Hunter DJ. Lumbar facet joint osteoarthritis: a review. Semin Arthritis Rheum. 2007;37(2):69-80.
- Reviews the anatomy, biomechanics, risk factors, and imaging of lumbar facet joint osteoarthritis. Shows that many people develop arthritis in the spinal joints as they age, but not all arthritis causes pain, which is why diagnosis requires careful assessment.
https://pubmed.ncbi.nlm.nih.gov/17379279/
2. Manchikanti L, Pampati V, Fellows B, Bakhit CE. Prevalence of lumbar facet joint pain in chronic low back pain. Pain Physician. 1999;2(3):59-64.
- Classic prevalence study using double diagnostic blocks, estimating that facet joints are the pain source in up to 45% of people with chronic low back pain. Shows why facet pain is common, why single injections are unreliable, and why controlled medial branch blocks matter for diagnosis.
https://pubmed.ncbi.nlm.nih.gov/16906217/
3. Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The false-positive rate of uncontrolled diagnostic blocks of the lumbar zygapophysial joints. Pain. 1994;58(2):195-200.
- Landmark study showing that single uncontrolled facet joint injections can produce false-positive results in many patients. Confirms why accurate diagnosis of facet joint pain relies on controlled medial branch blocks, not just one injection or scan, helping to avoid misdiagnosis and unnecessary treatments.
https://pubmed.ncbi.nlm.nih.gov/7816487/
4. Cohen SP, Huang JH, Brummett C. Facet joint pain – advances in patient selection and treatment. Nat Rev Rheumatol. 2013;9(2):101-116.
- Narrative review covering recognition of facet-mediated back pain, diagnostic accuracy, and treatment options including intra-articular steroid injections, medial branch blocks, and radiofrequency ablation. Emphasises patient selection, the limits of imaging, and the role of controlled diagnostic blocks before proceeding to radiofrequency.
https://pubmed.ncbi.nlm.nih.gov/23165358/
5. Dreyer SJ, Dreyfuss PH. Low back pain and the zygapophysial (facet) joints. Arch Phys Med Rehabil. 1996;77(3):290-300.
- Comprehensive review of facet joint anatomy, biomechanics, and referral patterns with clinical testing. Explains how facet-mediated back pain differs from disc or sacroiliac pain and why extension and rotation often aggravate symptoms.
https://pubmed.ncbi.nlm.nih.gov/8600875/
6. Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine. 2000;25(10):1270-1277.
- Seminal prospective audit showing that lumbar medial branch radiofrequency neurotomy provides long-term relief in carefully selected patients after controlled diagnostic blocks. Establishes key technical factors for needle placement that underpin modern practice.
https://pubmed.ncbi.nlm.nih.gov/10806505/
7. Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106(3):591-614.
- Detailed review of the mechanisms, diagnosis, and management of facet joint pain. Covers the limitations of imaging and the value of diagnostic medial branch blocks.