Migraine
When Migraine Takes Over Your Life
Migraine isn’t just a bad headache. It’s a debilitating neurological condition that can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It can take control of your day, your energy, your ability to think clearly and most of your life. For many, it’s invisible, and often misunderstood. People say things like “just take a tablet” or “you’ll be fine tomorrow”. But for those living with chronic or recurring migraine, it’s not that simple.
Migraine Aura Simulation - Zig-zag visual disturbance commonly reported before headache onset
You may be here because you’ve tried everything. You’ve been told to hydrate, avoid triggers, or rest. You’ve likely seen or have a neurologist or been prescribed multiple medications. And yet, the pain keeps coming, often with nausea, brain fog, vision changes or dizziness.
At Pain Specialists Australia, we treat people who live with migraine that won’t go away, chronic migraine. If standard treatments haven’t helped, we offer a new approach - one that combines advanced therapies with real listening and support.
MIgraine characteristics vs. Tension-Type Headache characteristics
What is migraine and how is it different from a headache?
Migraine is a chronic, severe and debilitating neurological condition that causes recurrent episodes of head pain and sensory sensitivity. It’s often accompanied by nausea, vomiting, visual disturbances (known as aura), and heightened sensitivity to light, sound or smell.
Unlike a regular tension headache, migraine is typically one-sided, pulsating, and can be severely disabling - affecting your ability to think, move, or function. Many people also experience fatigue, mood changes or brain fog before and after the pain itself, making migraine a full-body experience, not just a headache.
The exact cause of migraine isn’t fully understood, but it’s believed to involve a mix of genetic, neurological, and environmental factors. Changes in brain activity affect the way nerves communicate, how blood vessels function, and how the brain processes pain. Some people may have a heightened sensitivity in the brainstem and trigeminal nerve pathways, which can trigger the complex symptoms of a migraine attack.
Our Approach to Managing Migraine
We see you - not just your symptoms. Our migraine specialist treatment plans are tailored to people who feel stuck, worn down, and ready for something that actually helps.
Diagnosis and Assessment
We begin by hearing your story. When did the migraine begin? What triggers have you noticed? Have you been diagnosed with chronic migraine, migraine, or something less defined?
We review any relevant imaging, reports, or medication history. Migraine isn’t always a stand-alone issue, we often see it linked to neck pain, stress, hormonal cycles, poor sleep, or medication overuse. There are many triggers to consider. That’s why our team includes not just doctors, but physiotherapists, psychologists, and dietitians.
We work alongside your GP or neurologist - not in competition, but in support of them. Our role is to offer specialised and advanced pain management options that fit into your wider care plan.
Medication and Non-Medication Options
Sometimes medication is the right answer - and sometimes it makes things worse. Many of our patients arrive stuck in a loop of pain medications that no longer help. If medication hasn’t worked for you, we’ll consider options such as:
Preventive medications
Migraine attack treatment medications
Non-opioid rescue plans
Opioid weaning strategies
IV infusion therapies (for selected patients)
Our focus is always to reduce harm, increase function, and return control to you.
Nerve Blocks and Targeted Interventions
For people with persistent, treatment-resistant migraine, targeted procedures can block or modulate pain signals at their origin or along the nerve pathway. These interventional techniques are often used when medications have failed or caused intolerable side effects.
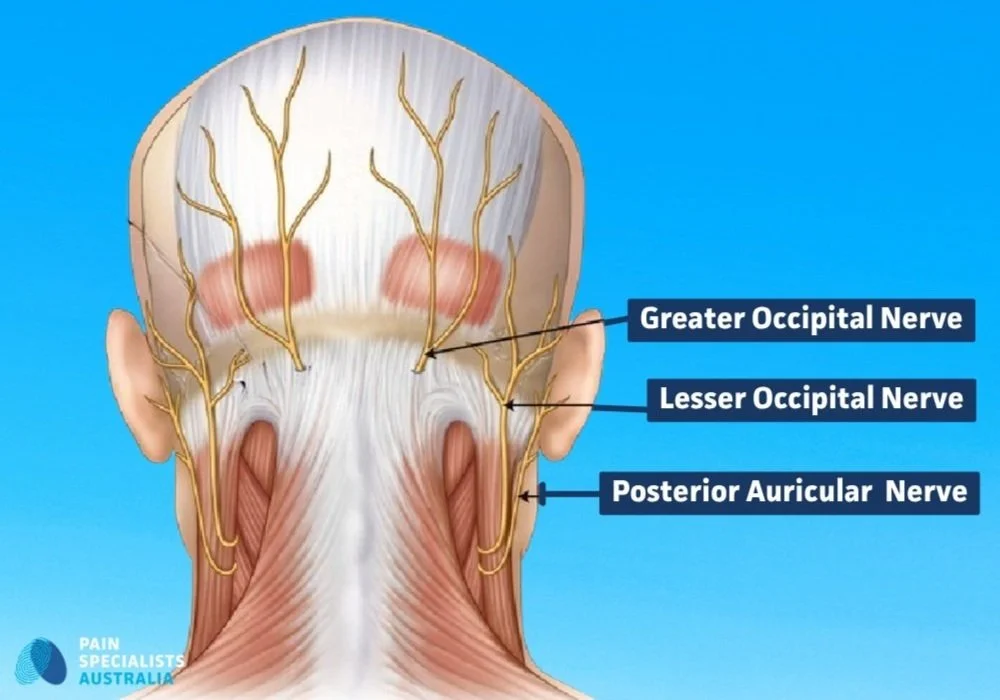
Occipital Nerves Targeted in Migraine Treatment
1. Occipital and Sphenopalatine Nerve Blocks
These simple, minimally invasive injections target the greater occipital nerve (GON) or the sphenopalatine ganglion (SPG) - two key hubs in migraine pathways. Blocking these nerves may reduce the frequency, duration and severity of migraine attacks, particularly in people who haven’t responded well to oral or injectable medications.
2. Pulsed Radiofrequency (PRF) to Greater Occipital Nerve and/or the sphenopalantine ganglion
Pulsed RF delivers low-intensity electrical energy to the GON or SPG, reducing nerve overactivity without damaging tissue. It’s a longer-lasting, non-destructive option for chronic daily migraine or medication-refractory migraine. Relief may last months or longer, and the procedure is repeatable if needed.
3. Neuromodulation and Occipital Nerve Stimulation
In severe, disabling migraine where other therapies have failed, neuromodulation may offer a solution. Occipital nerve stimulation involves placing a small, implantable device under the skin to gently stimulate the occipital nerves. This reduces abnormal pain signalling and can significantly improve quality of life in selected patients.
Lifestyle, Allied Health, and Team-Based Care
Migraine isn’t just a brain problem - it’s a whole-person condition. That’s why we take a team-based, integrated approach that looks beyond the pain to support every part of your system. At Pain Specialists Australia, our allied health team works closely with our pain specialists to tailor a management plan that’s built around you - your body, your lifestyle, and your goals.
We don’t offer one-size-fits-all solutions. We help you rebuild the foundation of wellness.
1. Physiotherapy
Our physios assess for neck-related (cervicogenic) triggers, postural strain, and muscle tension that may contribute to migraine attacks. Treatment may include education, empowerment, movement retraining and home-based exercises designed to reduce flare-ups and restore function.
2. Psychology
Migraine can be emotionally exhausting. Our psychologists offer strategies to manage the stress, anxiety, and isolation that often accompany chronic migraine. Techniques may include CBT, ACT, pacing support and resilience-building, all tailored to your lived experience.
3. Dietetics
Food triggers, fasting states, gut dysfunction, and even blood sugar swings can influence migraine patterns. Our dietitians can help identify potential dietary triggers, guide elimination protocols safely, and support better gut-brain health, without overly restrictive diets.
We don’t just treat the pain in your head. We care about the life you’re trying to live.
Why Choose Pain Specialists Australia?
Many people come to us after years of being told it’s all in their head - or after trying treatment after treatment with no real change. Here’s what makes us different:
We take you seriously - your symptoms, your language, your goals
We perform advanced treatments, including pulsed RF and neuromodulation
We work with your neurologist or GP, not in isolation
We tailor your care based on what you’ve already tried - and what is best for you
We use non-opioid, research-based methods to reduce pain and improve daily life
What Patients Tell Us
We’ve listened to hundreds of real stories - from clinic visits, online forums, and support groups - and the themes are strikingly consistent. These are not just medical symptoms; they are lived experiences that often go unrecognised and untreated. Here’s what we hear most often:
Migraine Mornings - Waking with Head Pain
“I’ve tried everything and nothing works.”
“No one believes how bad it really is.”
“I’m tired of being told to rest and drink water.”
“It’s not just the pain - it’s the fog and fear of the next one.”
“I just want a plan that makes sense for me.”
“My migraine won’t go away.”
“What helps migraine when nothing works?”
“I tried Botox but it made no difference.”
“I waited 9 months to see a neurologist and nothing changed.”
These aren’t just complaints - they’re quiet cries for better care. At Pain Specialists Australia, we listen closely, and we act decisively. We understand that migraine is more than just a headache. It’s a condition that affects your work, your relationships, your identity - and your hope.
That’s why we don’t stop at medication. We build tailored, multidisciplinary plans that consider your full experience - not just your scan results. Because when you feel heard, you’re already one step closer to healing.
Book Migraine Treatment in Melbourne
If you’re living with chronic migraine, it can feel like you’re going around in circles - trying medications, adjusting your routine, and still not getting the relief you need. But there are evidence-based treatments that go beyond standard care, especially when tailored to your specific situation.
Speak with your GP about a referral to Pain Specialists Australia. We work with you and your existing care team to explore next steps, with a focus on respect, expertise, and practical support.
Frequently Asked Questions (FAQ)
1. What is migraine and how is it different from a headache?
Migraine is a chronic neurological condition causing severe, recurring one-sided, pulsating head pain. It often includes nausea, vomiting, visual aura, and sensitivity to light, sound, or smell. Unlike tension headaches, migraines can be disabling and affect thinking, movement, and function, often with fatigue or brain fog before and after attacks.
2. What causes migraines?
The exact cause of migraines isn’t fully known but involves genetic, neurological, and environmental factors. Changes in brain activity affect nerve communication, blood vessel function, and pain processing. Some people have increased sensitivity in brainstem and trigeminal nerve pathways, triggering the complex symptoms of a migraine attack.
3. What are migraine triggers?
Migraine triggers are factors that can set off an attack in people who are prone to migraine.
Common triggers include stress, poor sleep, hormonal changes, certain foods or additives, dehydration, skipping meals, bright lights, strong smells, and weather changes.
Triggers vary from person to person, and identifying patterns is often an important step in managing migraine more effectively.
4. What treatments are available for migraine in Australia?
Chronic migraine treatment in Australia includes a combination of medical, interventional, and lifestyle-based approaches.
Options may include acute and preventive medications, nerve blocks, pulsed radiofrequency (RF) advanced procedures, physiotherapy, psychological therapy, dietary strategies, and in rare cases, neuromodulation.
The most effective treatment plans are tailored to each person and often involve a team-based approach that targets both the nervous system and contributing lifestyle factors.
5. What if migraine medication isn’t working for me?
Many people with chronic migraine find that standard or even new migraine medications don’t provide enough relief - or cause unwanted side effects. In these cases, targeted treatments such as nerve blocks, pulsed radiofrequency, or neuromodulation may help reduce pain and improve quality of life.
A multidisciplinary approach that includes physiotherapy, psychology, and lifestyle support can also play a vital role in managing migraine when medications alone fall short.
6. Can I still see my neurologist or GP?
Absolutely. Pain management works best when it’s part of a team effort. We collaborate closely with your GP, neurologist, or other specialists to ensure your care is seamless, coordinated, and comprehensive.
Our role is to bring in additional tools - like advanced interventional procedures, pain neuroscience education, and allied health support - to complement and enhance your existing treatment plan.
7. Are nerve blocks and neuromodulation safe for migraine?
Yes - these are well-established procedures with a strong safety record when performed by experienced pain specialists. Nerve blocks and neuromodulation are guided by imaging when needed and are used worldwide to treat complex or medication-resistant migraine.
While the risks are generally low, every procedure carries some potential side effects. These need to be carefully weighed against the severity of your symptoms, your response to previous treatments, and the overall impact migraine is having on your life. Discuss these with your migraine pain specialist.
These treatments aren’t suitable for everyone, but in carefully selected cases, they can lead to significant and lasting improvement.
8. Can migraine cause neck pain?
Yes - neck pain is a common symptom during or before a migraine attack. It may be caused by muscle tension, nerve sensitisation, or shared pain pathways between the neck and brain. For some people, neck pain can also act as an early warning sign (or “prodrome”) that a migraine is coming.
In others, neck problems may even trigger migraine-like symptoms, making diagnosis and treatment more complex.
If you’re not sure whether your neck pain is part of your migraine or something separate, it’s best to get assessed by a pain specialist.
9. When is a migraine dangerous?
Most migraines are not life-threatening, but certain warning signs should never be ignored. A migraine may be dangerous if it:
Comes on suddenly and severely. We call this a “thunderclap” headache
Feels different from your usual migraine pattern
Is accompanied by slurred speech, weakness, vision loss, or confusion
Follows a head injury
Occurs with fever, neck stiffness, or seizure
These could indicate a more serious condition, such as stroke, meningitis, or bleeding in the brain.
If you’re unsure or the symptoms feel unusual, it’s safest to seek immediate medical care.
READY FOR RELIEF?
References
Further Reading and References on Migraine and Headache Management:
1. Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017 Apr;97(2):553-622.
- This comprehensive review by world-leading migraine researchers details the neurobiological mechanisms underlying migraine, emphasising its nature as a disorder of sensory processing. It is widely cited and forms the scientific foundation for understanding migraine as a complex brain disorder, guiding both diagnosis and modern treatment approaches.
https://pubmed.ncbi.nlm.nih.gov/28179394/
2. Charles A. The pathophysiology of migraine: implications for clinical management. Lancet Neurol. 2018 Feb;17(2):174-182.
- This authoritative review synthesises emerging insights into migraine pathophysiology and directly links these mechanisms to practical treatment strategies. It is frequently referenced by clinicians seeking to apply the latest science to real-world migraine management.
https://pubmed.ncbi.nlm.nih.gov/29229375/
3. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache. 2015 Jan;55(1):3-20.
- This evidence-based guideline from the American Headache Society is a cornerstone reference for acute migraine therapy. It provides clear, graded recommendations on pharmacological treatments, supporting clinicians in delivering standard-of-care management.
https://pubmed.ncbi.nlm.nih.gov/25600718/
4. Lipton RB, Dodick DW, Silberstein SD, et al. Long-term safety and efficacy of erenumab in patients with episodic migraine: Results from a 5-year, open-label extension study. Cephalalgia. 2022 Feb;42(2):179-189.
- This pivotal long-term study demonstrates the sustained efficacy and safety of erenumab, a CGRP monoclonal antibody, for migraine prevention. It is a key reference for clinicians considering newer preventive therapies.
https://pubmed.ncbi.nlm.nih.gov/33400330/
5. Ashina M, Katsarava Z, Do TP, et al. Migraine: epidemiology and systems of care. Lancet. 2021 Apr 10;397(10283):1485-1495.
- This authoritative review discusses the global burden of migraine, barriers to diagnosis and treatment, and the need for improved healthcare systems. It is a go-to reference for understanding the public health impact of migraine and advocating for better patient care pathways.
https://pubmed.ncbi.nlm.nih.gov/33773613/
6. Blumenfeld AM, Silberstein SD, Dodick DW, et al. OnabotulinumtoxinA for chronic migraine: Pooled analyses of the PREEMPT clinical program. Headache. 2018 Feb;58(2):239-255.
- This pooled analysis of the landmark PREEMPT trials confirms the efficacy and safety of onabotulinumtoxinA (Botox) for chronic migraine. It is a foundational reference for interventional migraine management.
https://pubmed.ncbi.nlm.nih.gov/20487038/
7. Cady RK, Schreiber CP, Farmer KU. Nerve blocks and other interventional procedures for headache. Headache. 2010 Apr;50(4):623-7.
- This clinical review provides an overview of nerve blocks and related procedures for headache, including migraine. It is a practical resource for clinicians seeking interventional options beyond standard pharmacological therapy.