Trigeminal Neuralgia
At Pain Specialists Australia, we diagnose and treat trigeminal neuralgia (TN). We build a clear, stepwise plan: medication first, then where appropriate, image-guided procedures or surgical collaboration when needed.
Electric shock-like, one-sided facial pain set off by light touch or a breeze is frightening. Make sure you get the right expert treatment.
What Is Trigeminal Neuralgia?
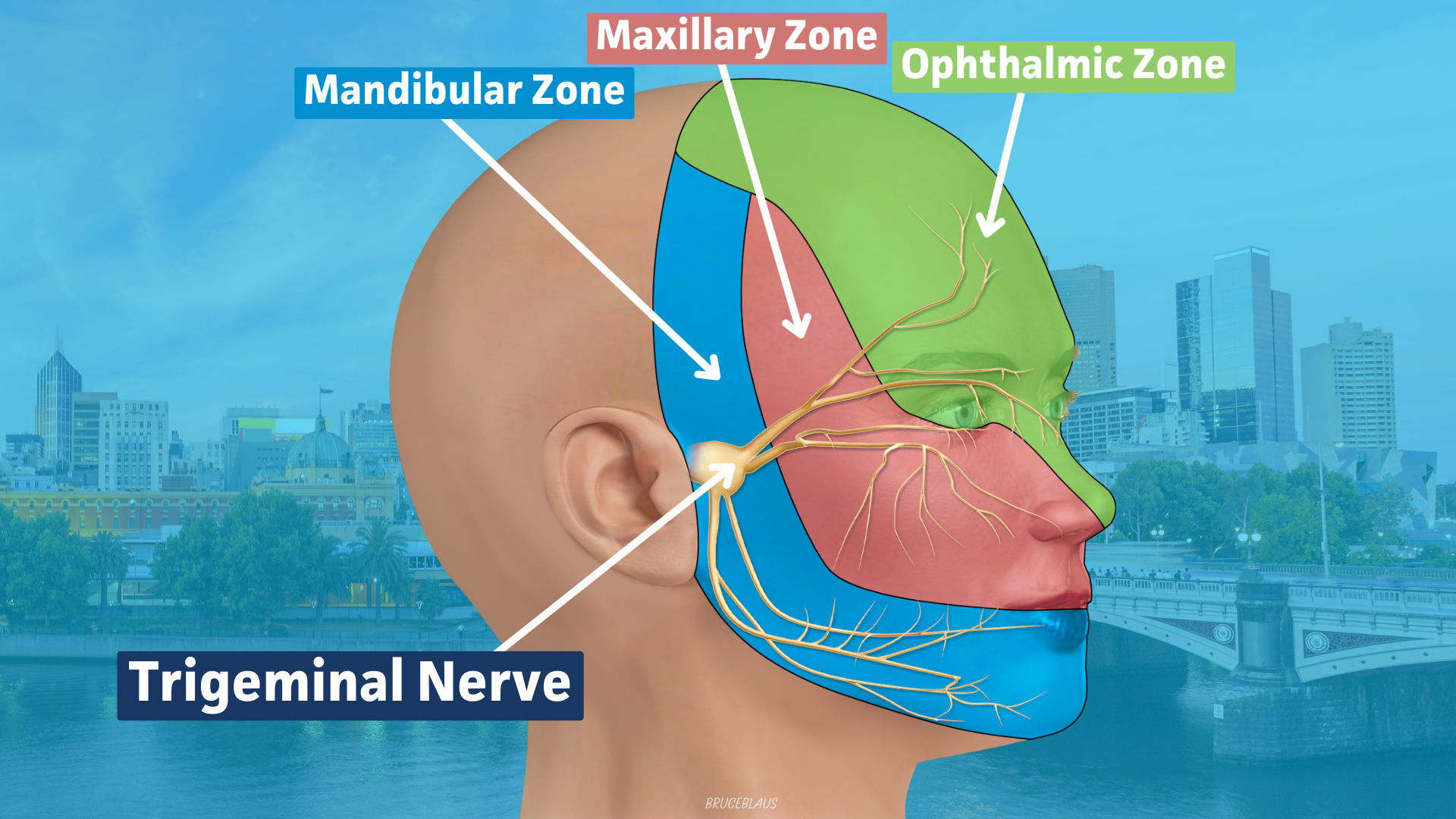
Trigeminal neuralgia causes brief, electric shock-like pain on one side of the face. Everyday touch - brushing, eating or a cool breeze - can trigger jolts. Diagnosis is clinical and often supported by MRI.
Treatment starts with medication, then progressing with image-guided or surgical options when needed.
Causes of Trigeminal Neuralgia (Why It Happens)
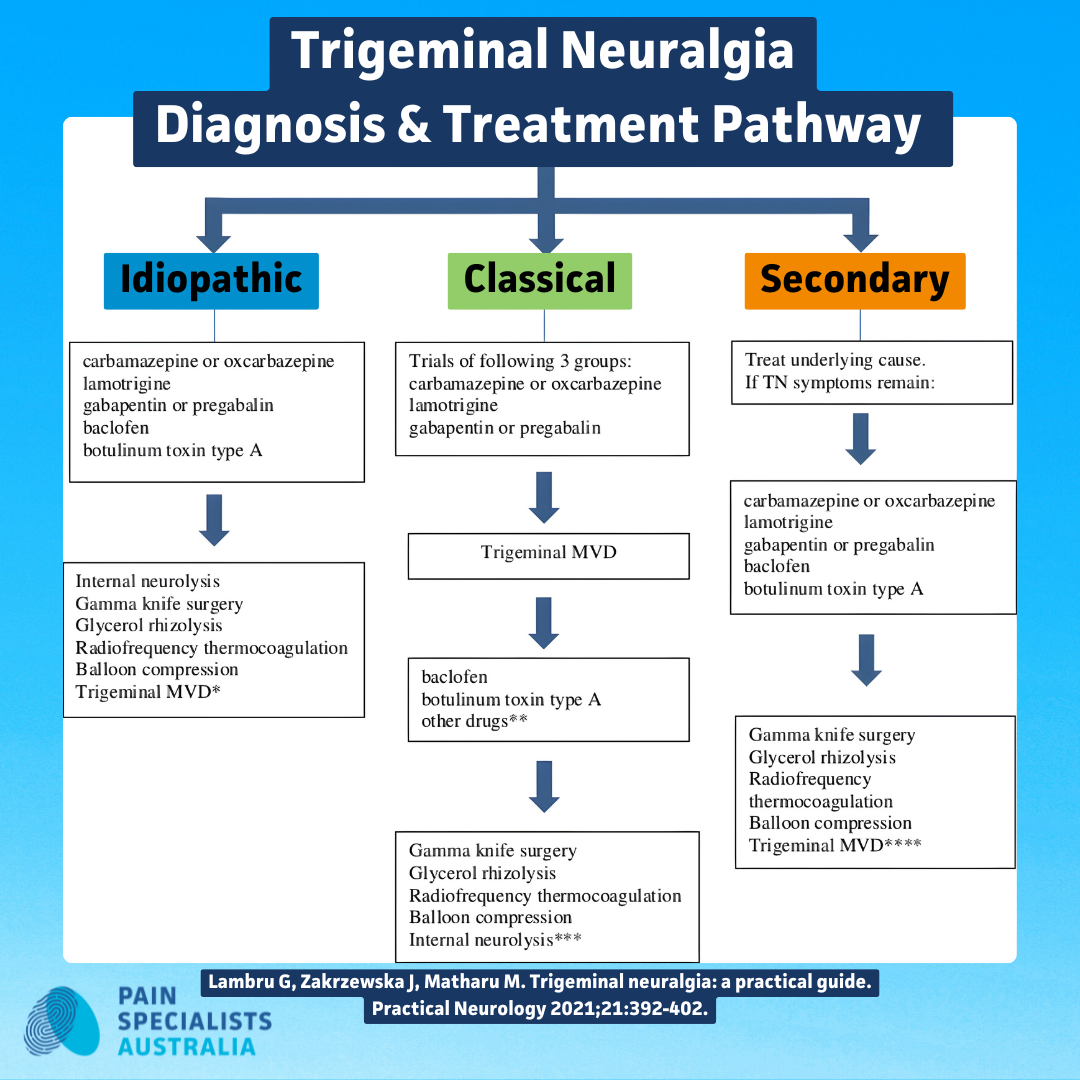
Most people with TN fit one of four patterns. Identifying yours helps us choose the safest, most effective pathway.
Classic TN (neurovascular compression)
In classic TN, a small artery or vein presses on the trigeminal nerve near the brainstem. This contact can irritate the myelin (insulation) and trigger shock-like pain from light touch. MRI may show vessel–nerve contact. In cases that don’t respond to medications, neurosurgeons may consider microvascular decompression (MVD). Other treatments might include image-guided procedures.
Secondary TN (due to another condition)
TN can be driven by an underlying issue such as multiple sclerosis (MS), tumour/cyst, or changes like scarring after prior surgery.
MS can create demyelinating plaques along the trigeminal pathway. Clues include facial numbness between attacks, continuous background pain, both sides being affected, or other neurological signs. We co-manage with neurology/neurosurgery when this pattern is suspected.
Idiopathic TN (no clear cause on tests or scans)
Your assessment points to TN but MRI doesn’t show compression or another cause. Care follows the standard pathway (medication first), with image-guided options or surgical collaboration if attacks persist.
Painful trigeminal neuropathy (not classic TN)
Here the nerve is injured or inflamed (e.g., facial trauma, dental/sinus procedures, shingles/post-herpetic, or persistent idiopathic facial pain).
People often report a more constant background discomfort with superimposed jolts. Options can include targeted peripheral nerve radiofrequency (supra/infraorbital, mental, mandibular), sphenopalatine ganglion (SPG) blocks, neuromodulation in selected cases, and tailored medication plans.
Why cause matters for your plan
Different causes of TN may have different treatment pathways. The right diagnosis is important.
Classic compression → medicines first; if needed, Gasserian Ganglion radiofrequency or balloon compression or glycerol neurolysis or discussion of MVD/radiosurgery with our partners.
Secondary TN (e.g., MS) → co-management with neurology; procedure selection and expectations may differ.
Neuropathy patterns → branch-targeted treatments (peripheral RF, SPG blocks) and realistic timelines.
Common Signs & Triggers People Report
Electric shock-like, one-sided facial pain
People describe intense, electric jabs lasting seconds to minutes, often in clusters. Between attacks, you may feel normal or mildly achy. Flares can come in waves, with pain-free periods in between.
Triggers: brushing, chewing, light touch, breeze, shaving, makeup
Typical triggers include toothbrushing, eating, speaking, smiling, washing the face, shaving or applying makeup, and even a gentle breeze. Triggers can sometimes help confirm diagnosis and guide the treatment path.
Everyday triggers for trigeminal neuralgia pain.
Is It TN or Tooth/Jaw Pain? (How to Tell & Who to See)
TN pain is usually one-sided, sudden, and shock-like, with clear touch triggers.
Dental/jaw problems tend to cause steady, aching, pressure-sensitive pain and usually have a trigger like a dental procedure.
If you’re unsure, we’ll examine you, review dental history, and coordinate with your GP, dentist, or oral-medicine specialist so you’re not bounced between providers.
Many people tell us they’ve seen dentists, neurologists, or GPs before finally getting the right diagnosis.
You’re not alone, TN is often misdiagnosed at first.
Your Melbourne Treatment Pathway
We start with a focused history and examination, check trigger zones/branches, and arrange an MRI if indicated. Then we move stepwise, matching options to your goals and medical context.
Diagnosis & initial medication plan (shared care)
First-line management typically uses anti-neuropathic (nerve) medicines (dosing and monitoring tailored to you), shared with your GP/neurologist to minimise side effects and interactions. Sometimes combinations of medications work better than a single medication.
When medication isn’t helping or not tolerated
When medications don’t help, or side effects get in the way, we step up to image-guided options that target pain pathways with precision. You’ll know benefits, risks and what to expect.
Image-Guided Options We Offer (When Medications Aren’t Enough)
Image-guided trigeminal procedure in a fluoroscopy suite.
Gasserian ganglion radiofrequency (continuous or pulsed)
Using X-ray guidance, or CT guidance, a fine electrode reaches the Gasserian ganglion (a relay of the trigeminal nerve). Continuous RF carefully heats a pinpoint area to interrupt pain signals; pulsed RF modulates the nerve with lower thermal effect. Aim: rapid relief while balancing sensation changes. Typically done as a day-procedure with sedation.
Balloon compression vs glycerol rhizolysis (selection & expectations)
Both approaches target the gasserian ganglion via a tiny needle pathway. Balloon compression briefly inflates a soft balloon to compress pain fibres; glycerol neurolysis uses a small amount of glycerol to disrupt pain transmission. Choice depends on your pain pattern, imaging, and preferences. We work with expert facial pain/TN neurosurgeons who deliver this therapy for you. Expect immediate or early relief for many; some facial numbness or tingling is possible and as always risks vs. benefits are considered.
Peripheral nerve RF (supra/infraorbital, mental, mandibular) & SPG blocks
When pain is branch-predominant or atypical, peripheral nerve RF can target the specific branch (e.g., supra/infraorbital, mental). SPG blocks may help selected patients with facial pain flares. These can be diagnostic (confirm the right nerve) and therapeutic and may be repeated if benefit wanes.
Who benefits, potential risks, and realistic timeframes
Who benefits: Classic, triggerable TN not controlled by medication; branch-predominant facial pain; people preferring minimally invasive options or unsuitable for open surgery like MVD.
Risks we discuss: Temporary soreness, altered facial sensation or numbness, rare bleeding/infection; procedure-specific risks explained in plain English.
Timeframes: Relief may be immediate or develop over days; durability varies and we plan follow-up and revisit options if pain returns.
After MVD: What If Pain Comes Back?
Review, imaging, and next steps in Melbourne
Recurrence after microvascular decompression (MVD) happens for some. We’ll work with your neurosurgeon and review your operative history, examine trigger zones, and repeat imaging if needed. From there, we’ll map options that suit your history, from medications to percutaneous RF and and even coordination with neurosurgeon to understand if a repeat operation should be considered.
Considering radiosurgery or repeat procedures with our partners
If you are considering these options, we’ll support your team as needed. If you don’t have a neurosurgical team, we’ll support and arrange this for you.
Why Choose Pain Specialists Australia?
We are one of the premier pain clinics in Australia. With decades of expertise and experience in complex pain diagnosis and treatment. Our specialist doctors are globally trained and have the network of specialists ready to support you.
Team approach with neurology & neurosurgery partners
You get a coordinated plan, not a single procedure in isolation, we work with your GP, dentist/oral medicine specialist, neurologist, and neurosurgeon.
Evidence-based interventional care with clear follow-up plans
We use established techniques, careful dosing/lesioning, and structured follow-up so you know what to expect and when to check in.
What Patients Describe (Common Experiences)
“I avoid brushing or talking for fear of a jolt”
Fear of triggers drives avoidance. We design plans that reduce flare risk and restore everyday routines.
“Side effects from meds were tough; I want options”
When tablets help but cost too much in side effects, or simply don’t help, we step through minimally invasive choices considering risks vs benefits.
“I need a plan that makes sense, and fast”
We prioritise clarity: what it is, what happens next, and how we’ll measure progress.
When to Escalate Urgently (Safety First)
If pain is escalating or you’re unable to eat, drink, or take medicines, seek urgent care via your GP, or Emergency Department, or 000. If you feel overwhelmed or unsafe, please reach out to crisis supports. Your safety comes first.
For national support, visit the Trigeminal Neuralgia Association Australia (TNAA).
Frequently Asked Questions (FAQ)
1. Who treats trigeminal neuralgia in Melbourne?
In Melbourne, trigeminal neuralgia is usually managed by pain specialists and neurosurgeons working together.
2. Why do brushing, shaving or a breeze trigger electric-shock pain?
In TN, touch and temperature changes can set off hyper-excitable facial-nerve fibres, causing sudden jolts, which can literally stop people in their tracks as they walk, sometimes even dropping to the ground in excruciating pain.
3. How do I tell TN from a dental/tooth problem?
TN: brief, shock-like, one-sided, clearly triggerable.
Tooth/jaw: steady ache, pressure-sensitive, often tender on biting. We’ll examine you and coordinate dental input if needed.
4. What if medication isn’t helping or causes side effects?
We discuss Gasserian RF (continuous/pulsed), balloon compression, glycerol neurolysis, and targeted peripheral nerve options, matching pros/cons to your goals.
5. I’ve had MVD and the pain is back, what now?
We’ll review your story and imaging, then outline options that might include percutaneous options, radiosurgery, or neurosurgical review for possible re-operation.
6. Do radiofrequency procedures numb my face?
Some approaches can cause temporary or longer-lasting altered sensation. We explain likelihoods, safety steps, and why small trade-offs can bring big relief for some.
7. How quickly could I get relief?
Some procedures relieve pain quickly; others (like radiosurgery) can take longer to help. We’ll give you realistic timelines for each option.
8. Is TN curable or mainly managed over time?
Many achieve excellent control particularly with MVD. Durability varies by option and individual factors; we plan follow-up and revisit choices if pain changes.
9. Can TN be part of multiple sclerosis (MS)?
Yes. Pathways and procedure selection may differ; we coordinate with your neurologist or if you don’t have one, arrange one for you.
10. When should I seek urgent help?
If attacks are uncontrolled, you can’t maintain fluids/meds, or you feel unsafe, escalate care urgently.
11. What scans do I need if you suspect TN?
Usually an MRI of the brain with a dedicated trigeminal nerve protocol is arranged to check fo nerve compression, structural causes, or secondary conditions.
12. How long does relief last after radiofrequency for TN?
Relief often lasts 6 months to 3 years on average, depending on technique and nerve response, with review and repeat treatment as needed.
Next Steps in Melbourne
You deserve fast clarity and a plan that fits your life.
If TN is suspected or you’re living in fear of the next jolt we’ll help you move forward with confidence.
References
Further Reading and References on Trigeminal Neuralgia:
1. Cruccu G, Di Stefano G, Truini A. Trigeminal neuralgia. N Engl J Med. 2020;383:754–762.
- Authoritative NEJM review covering clinical features, differential diagnosis, MRI use for neurovascular compression, and a stepwise management approach: carbamazepine/oxcarbazepine first line, with MVD, percutaneous rhizotomy, glycerol/balloon procedures and radiosurgery as options. Clear notes on expectations, risks and recurrence.
https://pubmed.ncbi.nlm.nih.gov/32813951/
2. Bendtsen L, Zakrzewska JM, Abbott J, et al. EAN guideline on trigeminal neuralgia. Eur J Neurol. 2019;26:831–849.
- European Academy of Neurology guideline detailing diagnostic work-up and graded recommendations: first-line sodium channel blockers; MVD recommended for classical TN with compression; percutaneous procedures or radiosurgery for non-surgical candidates or refractory cases.
https://pubmed.ncbi.nlm.nih.gov/30860637/
3. Headache Classification Committee of the IHS. The International Classification of Headache Disorders, 3rd edition (ICHD-3). Cephalalgia. 2018;38:1–211. PMID: 29368949.
- Definitive diagnostic criteria distinguishing classical, secondary and idiopathic TN; emphasises brief, unilateral, electric shock-like paroxysms, trigger zones, and the role of precipitating stimuli. Forms the taxonomy underpinning research and clinical coding.
https://pubmed.ncbi.nlm.nih.gov/29368949/
4. Bendtsen L, Zakrzewska JM, Heinskou TB, et al. Advances in diagnosis and management of trigeminal neuralgia. Lancet Neurol. 2020;19:784–796.
- Contemporary review highlighting imaging advances, prognostic factors, and comparative outcomes of medical, percutaneous, radiosurgical and microvascular approaches; includes practical treatment algorithms and patient-centred decision points.
https://pubmed.ncbi.nlm.nih.gov/32822636/
5. Maarbjerg S, Di Stefano G, Bendtsen L, Cruccu G. Trigeminal neuralgia: diagnosis and treatment. Cephalalgia. 2017;37:648–657.
- Concise overview of clinical recognition, red flags for secondary causes, MRI protocols, and evidence-based therapy sequencing from medications through interventional and surgical options.
https://pubmed.ncbi.nlm.nih.gov/28076964/
6. Bick SKB, Eskandar EN. Surgical treatment of trigeminal neuralgia. Neurosurg Clin N Am. 2017;28:429–438.
- Surgical review focused on technique selection, efficacy and complications of MVD, percutaneous rhizotomy (RF, glycerol, balloon) and stereotactic radiosurgery; includes counselling points on durability and sensory change.
https://pubmed.ncbi.nlm.nih.gov/28600016/
7. Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ. 2015;350:h1238.
- Practical clinical review for primary and specialist care: presentation patterns, differential diagnosis with dental and TMJ pain, initial pharmacotherapy, and when to refer for image-guided or surgical treatment.
https://pubmed.ncbi.nlm.nih.gov/25767102/
8. llam AK, Sharma H, Larkin MB, Viswanathan A. Trigeminal neuralgia: diagnosis and treatment. Neurol Clin. 2023;41:107–121.
- Recent comprehensive update covering evaluation (including MRI protocols), pharmacological options, interventional techniques and surgical strategies; addresses special populations such as MS-associated TN and outlines follow-up/recurrence management.