Knee Pain Treatments in Melbourne
Understanding Knee Pain
Knee pain is a widespread problem that affects people of all ages, from active teenagers to older adults managing chronic conditions. It can range from a mild annoyance to a debilitating condition that interferes with daily life.
Whether your pain stems from a sports injury, wear-and-tear, or nerve-related issues, it can seriously impact your ability to walk, drive, exercise, sleep, or work productively. For many people, knee pain also limits social and recreational activities, leading to frustration, reduced mobility, and even low mood.
In some cases, knee pain begins suddenly after a fall or twist. Other times, it creeps in slowly over weeks or months. Regardless of how it starts, getting an accurate diagnosis is key to finding relief, especially if your pain has become persistent or is affecting your quality of life.
Common Causes of Knee Pain
Comparison of a healthy joint and an osteoarthritic knee with cartilage damage and a rheumatoid arthritis joint with inflammation
Joint Related Knee Pain
Joint problems are one of the most common causes of knee pain, often linked to inflammation, cartilage damage, or joint degeneration.
Osteoarthritis (wear and tear)
Rheumatoid arthritis
Gout and pseudogout
Septic arthritis (infection)
Injuries and Overuse
Injuries and overuse are frequent causes of knee pain, particularly in active individuals and athletes, where sudden movements or repetitive stress can damage key structures in the joint.
ACL and ligament tears
Meniscus tears
Patellar tendonitis and dislocations
Knee bursitis
Referred or Neuropathic Pain
Not all knee pain originates in the knee. Sometimes, it’s referred from the spine, hips, or nerves, leading to pain that feels deep, radiating, or out of proportion to local findings.
Spinal conditions (e.g., lumbar stenosis)
Nerve entrapments (e.g., meralgia paresthetica)
Post-herpetic neuralgia
Referred pain from hip or foot
Sensitisation & Chronic Pain
In some cases, ongoing knee pain is driven by sensitisation — a nervous system response where pain signals become amplified, leading to widespread discomfort even after the original injury has healed.
Nerve hypersensitivity
Pain spreading beyond the original injury
Sensitive skin, burning, or tingling sensations
Post-Surgical Knee Pain
While surgery can help repair structural damage, some people continue to experience knee pain long after the procedure - often due to nerve injury, inflammation, or scarring. This type of pain is different from mechanical joint pain and often requires specialist pain assessment.
Persistent pain after knee replacement or arthroscopy
Possible nerve injury, inflammation, or scarring
Up to 25% of knee surgeries may result in chronic pain
Who Is at Risk for Knee Pain?
Ageing adults
Athletes in high-impact sports
Sedentary individuals or those with poor fitness
People with physically demanding jobs
What Are the Symptoms of Knee Pain?
Knee pain can feel different depending on the cause. It might come on suddenly after an injury or build up slowly over time. Recognising the symptoms can help guide diagnosis and treatment.
Common Knee Pain Symptoms
Sharp, stabbing, or dull aching pain in or around the knee
Stiffness or reduced ability to bend or straighten the knee
Swelling or fluid build-up
Clicking, grinding, or crunching sounds (crepitus)
Weakness or the feeling of the knee “giving way”
Tingling, numbness, or pins and needles
Redness, warmth, or fever (if infection is present)
Radiating or Referred Pain
Pain that starts in the hip, thigh, or lower back and travels to the knee
Discomfort that worsens with walking, bending, or climbing stairs
Symptoms Suggesting Nerve Involvement
Burning or electric-shock sensations
Pain that spreads down the leg
Pain worse at night or with touch
Pain linked to previous shingles or nerve injury
Diagnosing Knee Pain
When to See a Specialist
Not all knee pain needs a specialist, but if your symptoms aren’t improving, it’s time to take a closer look.
You should consider seeing a pain specialist if:
Your knee pain has lasted longer than three months
The pain is keeping you up at night or limiting your ability to move
You experience weakness, instability, or the knee “giving way”
The pain radiates down your leg, feels electrical, or is accompanied by tingling or numbness
These symptoms could indicate nerve involvement, joint related pain, or other complex pain conditions that need more than rest and over-the-counter medication. A pain specialist can assess the underlying causes and offer targeted, non-surgical treatments to help you get back on track.
How Knee Pain is Diagnosed
Accurate diagnosis is the first step toward effective treatment. Your doctor or pain specialist will begin with a detailed clinical assessment, asking about your pain history, physical limitations, and any past injuries or surgeries.
Clinical Examination
A hands-on examination will assess:
Joint movement and range of motion
Muscle strength and stability
Areas of tenderness, swelling, or stiffness
Neurological function (e.g., sensation, reflexes)
This helps determine whether the pain is coming from the joint itself, surrounding soft tissues, or nerves.
Medical Imaging
Depending on the findings, your specialist may order imaging studies such as:
X-rays to detect joint changes like arthritis or bone spurs
Ultrasound to visualise soft tissues and inflammation
CT or MRI scans to assess cartilage, ligaments, menisci, or spinal structures
Imaging provides a clearer picture of what’s happening inside the knee or beyond it, if nerve or referred pain is suspected.
Treatments for Knee Pain
Acute Knee Pain
Acute knee pain usually develops suddenly — often after an injury or strain — and can often be managed with simple, short-term treatments to reduce inflammation and support healing.
Rest, ice, elevation
Simple pain relief and anti-inflammatories
Physiotherapy and gentle activity
Chronic Knee Pain
Chronic knee pain lasts longer than three months and often requires a more comprehensive approach; combining medical treatment, rehabilitation, and expert support to restore function and quality of life.
Chronic knee pain often persists even when scans appear normal.
Multimodal therapy combining physical and psychological rehab
Pain education and pacing strategies
Ongoing care from a specialist pain team
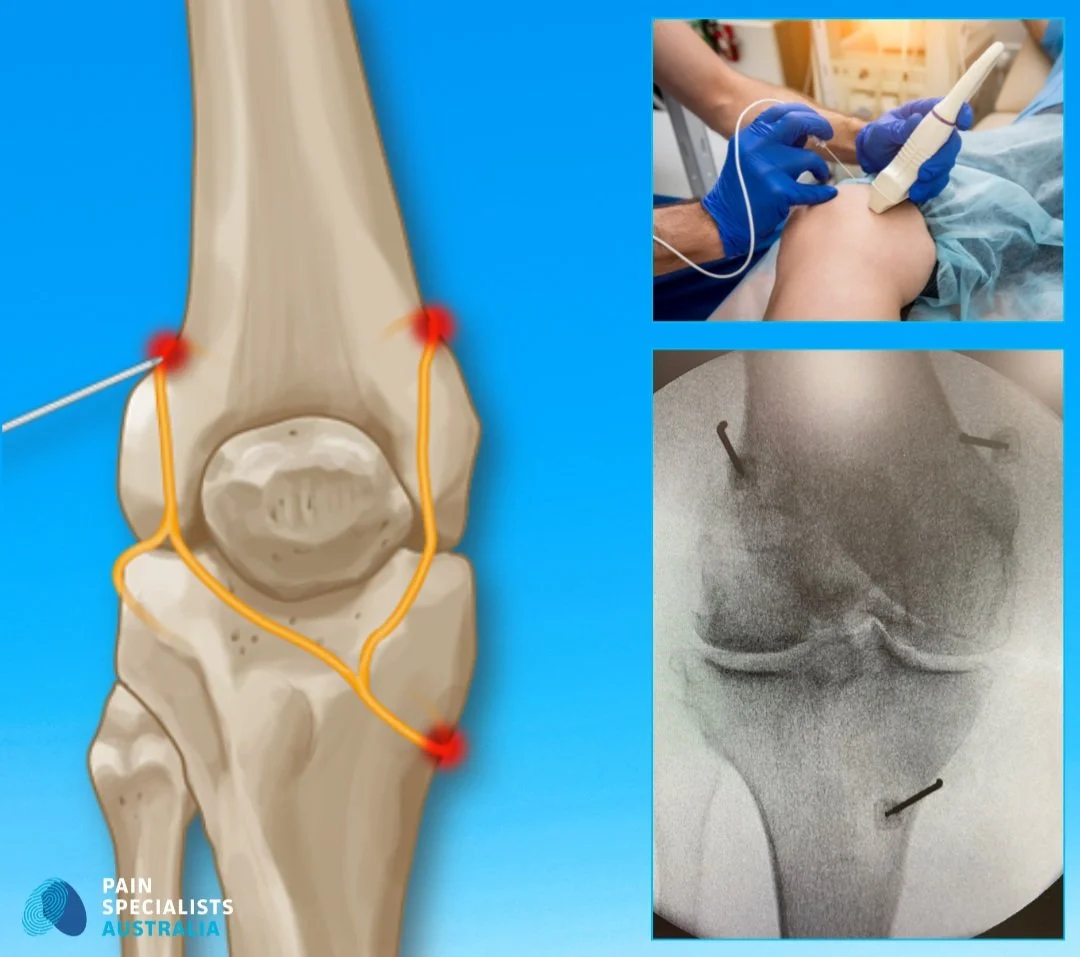
Radiofrequency ablation for knee arthritis pain relief
Interventional Pain Procedures
Interventional procedures can play a key part of managing persistent knee pain, especially when medications or physiotherapy alone haven’t worked. These targeted treatments, such as image-guided injections, nerve blocks, and radiofrequency ablation, can provide significant, lasting relief by addressing pain at its source.
Injections: steroid, platelet-rich plasma (PRP), genicular nerve blocks
Radiofrequency ablation (RFA), pulsed radiofrequency (PRF)
Advanced Therapies
For complex or treatment-resistant knee pain, advanced therapies like neuromodulation and sympathetic blocks may be recommended. When structural issues are suspected surgical intervention, we collaborate closely with some of Melbourne’s leading orthopaedic surgeons to ensure seamless, multidisciplinary care.
Neuromodulation: spinal cord stimulation
Referral for orthopaedic surgery if structural damage is present
LEARN MORE ABOUT OUR TREATMENTS
How to Get Knee Pain Relief in Melbourne
Getting relief from knee pain in Melbourne often starts with your GP, followed by a referral to a pain specialist who can coordinate expert care with physiotherapists, rehabilitation providers, and, when needed, surgeons.
Visit your GP for an initial assessment
Get a referral to a Pain Specialist for ongoing or worsening pain
Work with a team including physiotherapists and rehabilitation experts
When to Seek Urgent Help
If you experience one or more of the following symptoms, seek urgent medical attention:
Sudden, severe, or unrelenting pain
Inability to walk, bend, or bear weight
Swelling with fever, chills, or recent surgery
Signs of fracture or infection
Frequently Asked Questions (FAQ) - Knee Pain in Melbourne
1. What’s the most common cause of knee pain in adults?
Knee pain in adults can have many causes, including joint wear and tear, previous injury, overuse, or nerve-related pain. While osteoarthritis is common in older adults, not all knee pain is caused by arthritis, and many people have ongoing pain despite minimal changes on scans.
2. How do I know if my knee pain is serious?
If your pain lasts more than a few weeks, or is accompanied by swelling, warmth, instability, or limited movement, it’s worth seeing a specialist. These symptoms may indicate a more serious condition like infection, fracture, or nerve involvement.
3. Can chronic knee pain be treated without surgery?
Yes, many people with chronic knee pain improve with non-surgical treatments like nerve blocks, PRP injections, radiofrequency ablation, physiotherapy, and neuromodulation. Surgery is only recommended when there is clear structural damage that hasn’t responded to conservative care.
4. Do I need a referral to see a knee pain specialist in Melbourne?
Yes, most pain specialists require a referral from your GP to access Medicare rebates and ensure coordinated care. This also allows your GP to rule out serious conditions and refer you to the right specialist if needed.
5. What if I’ve had surgery but still have pain?
Persistent pain after knee surgery can be caused by nerve irritation, scar tissue, or unresolved inflammation. A pain specialist can help identify the underlying cause and offer advanced treatments to reduce pain and improve function.
6. Is it normal to have knee pain years after an injury or surgery?
Unfortunately, it’s not uncommon for people to experience long-term knee pain due to nerve sensitisation, joint degeneration, or post-surgical complications. This is not ok and requires assessment and treatment.
A thorough assessment with a pain specialist can help uncover the cause and guide effective treatment.
READY FOR RELIEF?
References
If you’re interested in more, here are some references for your perusal.
1. Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2012 Feb;42(2):81-94.
- This systematic review identifies overuse, biomechanical factors, and muscle imbalances as key risk factors for developing patellofemoral pain syndrome, especially in active populations.
https://pubmed.ncbi.nlm.nih.gov/22031622/
2. Hunter DJ, March L, Chew M. Osteoarthritis in 2020 and beyond: a Lancet Commission. Lancet. 2020 Nov 28;396(10264):1711-1712.
- This Lancet Commission highlights the growing global burden of osteoarthritis and calls for a shift toward prevention, personalised care, and non-surgical treatment options.
https://pubmed.ncbi.nlm.nih.gov/33159851/
3. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618-25.
- This landmark paper outlines how persistent post-surgical pain affects up to 25% of patients and identifies nerve damage and poor pain control as major risk factors.
https://pubmed.ncbi.nlm.nih.gov/16698416/
4. Duong V, Oo WM, Ding C, Culvenor AG, Hunter DJ. Evaluation and Treatment of Knee Pain: A Review. JAMA. 2023 Oct 24;330(16):1568-1580. doi: 10.1001/jama.2023.19675. PMID: 37874571.
- This JAMA review provides an updated overview of knee pain diagnosis, evaluation and treatment.
https://pubmed.ncbi.nlm.nih.gov/37874571/
5. Mo L, Jiang B, Mei T, Zhou D. Exercise Therapy for Knee Osteoarthritis: A Systematic Review and Network Meta-analysis. Orthop J Sports Med. 2023 Jun 5;11(5):23259671231172773.
- This review found that all exercise types improved symptoms in knee osteoarthritis, with aquatic exercise most effective for pain relief and yoga best for joint stiffness, function, and quality of life.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10280533/
6. Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, Crossley KM. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 2019 Oct;53(20):1268-1278.
- This systematic review found that MRI features of knee osteoarthritis are common even in asymptomatic, uninjured adults - appearing in up to 43% of those over 40 - highlighting the need to interpret imaging results alongside clinical symptoms.
https://pubmed.ncbi.nlm.nih.gov/29886437/
7. Ohashi Y, Uchida K, Fukushima K, Inoue G, Takaso M. Mechanisms of Peripheral and Central Sensitization in Osteoarthritis Pain. Cureus. 2023 Feb 22;15(2):e35331.
- This review outlines how peripheral and central sensitisation - driven by inflammatory cytokines, nerve growth factor, and serotonin - contribute to osteoarthritis pain, often independent of structural changes, highlighting emerging therapeutic targets.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9949992/
8. Bennell KL, Bayram C, Harrison C, Brand C, Buchbinder R, Haas R, Hinman RS. Trends in management of hip and knee osteoarthritis in general practice in Australia over an 11-year window: a nationwide cross-sectional survey. Lancet Reg Health West Pac. 2021 Jun 9;12:100187.
- Bennell et al. (2021) found that despite rising GP encounters for hip and knee OA in Australia, first-line lifestyle treatments remain underused, with ongoing reliance on imaging and medications.