Degenerative Disc Disease: Causes, Symptoms & Treatment
Stages of a disc herniation
What Is Degenerative Disc Disease?
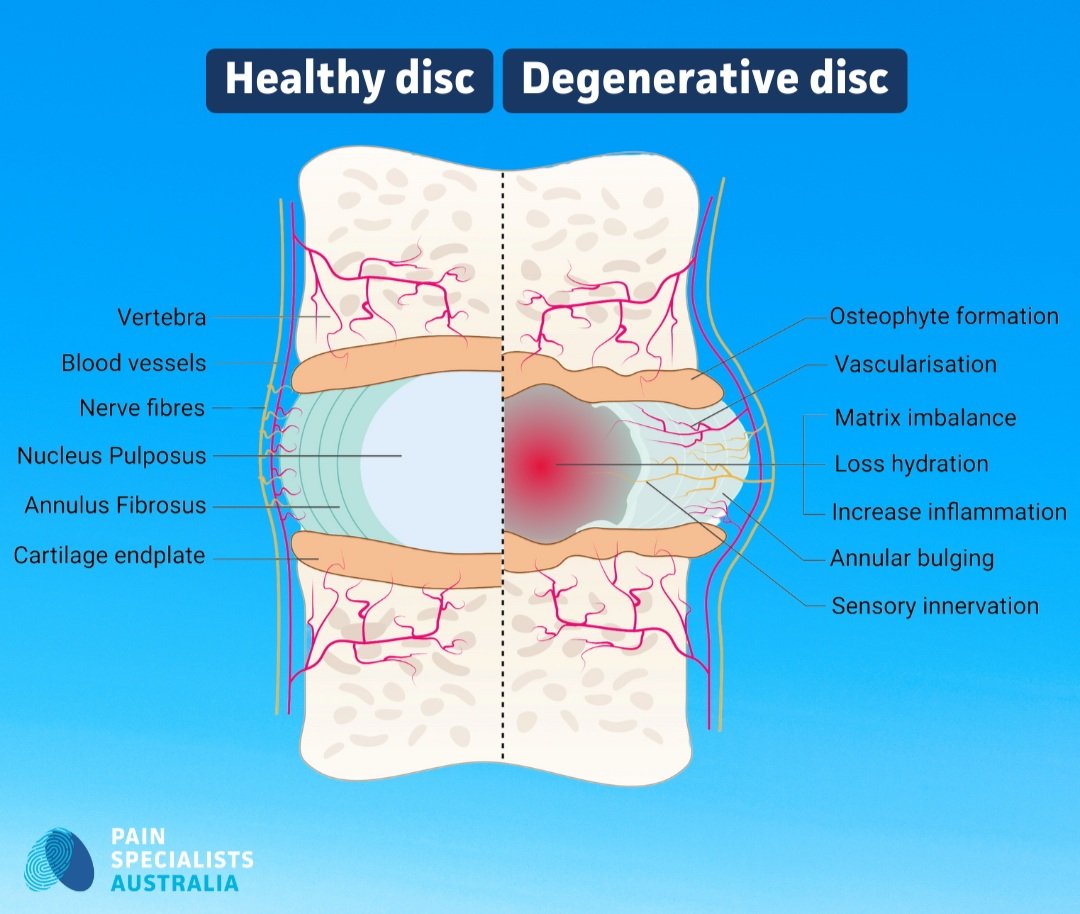
Degenerative disc disease (DDD) happens when the soft discs between your spine’s bones start to wear out. These discs work like shock absorbers - they keep your spine flexible and help protect it during everyday movements like walking, twisting, or lifting.
Over time, the discs can flatten, dry out, or lose their shape. When this happens, they don’t cushion the spine as well, and the bones may start to rub or shift.
This can lead to pain, stiffness, and less range of motion in your back or neck. In some cases, the disc may bulge or press on a nearby nerve, causing pain that travels into the legs or arms.
Illustration of a healthy vs. a degenerative disc
Mohd Isa, IL et al. Discogenic Low Back Pain: Anatomy, Pathophysiology and Treatments of Intervertebral Disc Degeneration. Int. J. Mol. Sci. 2023, 24, 208.
What Causes Degenerative Disc Disease?
The most common cause of disc degeneration is ageing. As we get older, the discs naturally lose water and become less spongy, which makes them more vulnerable to wear and tear. But age isn’t the only factor.
Repetitive stress such as heavy lifting, poor posture, or high-impact sports can speed up the breakdown of spinal discs. Past injuries like falls or car accidents can also play a role.
Genetics matter too; some people inherit a higher risk of disc problems. Lifestyle choices like smoking, lack of exercise, or being overweight can reduce blood flow to the discs, making them less healthy and more likely to degenerate.
Common Symptoms to Look Out For
Degenerative disc disease can cause a range of symptoms, and they don’t always stay the same from day to day. For many people, the most common sign is:
A dull or aching pain in the lower back or neck that gets worse with movement, especially bending, lifting, or sitting for long periods.
You might also feel numbness, tingling, or even weakness in your arms or legs. This can happen when a worn or bulging disc irritates nearby spinal nerves.
Other symptoms include:
Reduced flexibility and stiffness, making it harder to twist, bend, or get up from a seated position.
Some people notice that their pain improves when walking, lying flat, or changing position, especially after being still for a while.
These symptoms can come and go or gradually worsen over time. They may interfere with work, sleep, and simple everyday tasks, which is why early treatment is so important.
How Is Degenerative Disc Disease Diagnosed?
Diagnosing degenerative disc disease starts with a detailed conversation about your symptoms and medical history. Your doctor will ask when the pain started, what makes it worse or better, and how it affects your daily life.
A physical examination checks for things like muscle strength, flexibility, reflexes, and signs of nerve involvement. This helps your doctor understand how your spine is functioning and whether specific areas are irritated or weak.
Imaging tests like MRI or CT scans are often used to confirm the diagnosis. These scans provide detailed views of the discs, joints, and nerves in your spine. They help identify disc wear, bulging, or thinning and rule out other causes of pain like fractures, tumours, or infections.
Getting the right diagnosis is the first step in creating a personalised treatment plan that targets the actual source of your pain.
Non-Surgical Treatment Options
Specialist Physiotherapy improves strength, mobility, and spinal support.
Physical Therapy and Movement Plans
Tailored exercise programs play a key role in managing degenerative disc disease. A physiotherapist will assess your movement, pain triggers, and posture, then design exercises that suit your needs and abilities.
The focus is often on building strength in your core, hips, and back; the muscles that support your spine. Improving flexibility and posture helps reduce pressure on the affected discs, which can ease pain and prevent flare-ups.
Exercises might include gentle stretching, stabilising movements, and low-impact activities like walking or swimming. Over time, staying active this way can help you move more freely and get back to doing what you enjoy.
Pain Medications and Anti-Inflammatories
Pain from degenerative disc disease often includes both muscle and nerve involvement. Medications can help reduce discomfort, ease muscle tension, and improve how you move throughout the day.
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to lower inflammation in the spine and surrounding tissues. Muscle relaxants may be added if spasms are part of the problem, especially during flare-ups.
When nerve pain is present, for example, shooting pain down the leg, anti-neuropathic medications can help. They work by calming overactive nerves and are often used when symptoms feel sharp, burning, or tingling.
All medications should be used under medical guidance, as part of a larger treatment plan tailored to your condition and lifestyle.
Image-Guided Injection Therapies
Epidural steroid injections and nerve blocks offer targeted relief for inflammation and nerve-related back pain. These procedures are performed under live imaging, such as ultrasound or fluoroscopy, to ensure accuracy and safety.
They help reduce swelling around irritated nerves and interrupt the pain signals travelling to your brain. This can make movement easier and improve your ability to take part in physiotherapy or everyday tasks.
In some cases, more advanced options may be used. Radiofrequency ablation (RFA) is a technique that uses heat to block pain signals from spinal nerves, offering longer-lasting relief for facet joint or medial branch-related pain.
For patients with disc-related pain, procedures like intradiscal biaculoplasty may be considered. This minimally invasive treatment delivers radiofrequency energy directly into the damaged disc to calm nerve endings and reduce pain. These options are typically recommended when standard treatments haven’t provided enough relief, and are tailored to each patient’s specific condition.
Lifestyle Modifications and Self-Care
Maintaining a healthy weight, practicing good posture, and staying active. These changes can slow disc degeneration and improve overall spine health.
LEARN MORE ABOUT OUR TREATMENTS
When Is Surgery Recommended for Degenerative Disc Disease?
Surgery is considered when non-surgical treatments fail to relieve pain, or if there’s significant nerve compression causing weakness or loss of function.
It’s also an option when pain severely limits daily activities and quality of life.
What Are the Surgical Options for Degenerative Disc Disease?
Spinal Fusion: Joining two or more vertebrae to eliminate movement and reduce pain. This procedure stabilises the spine but may limit flexibility.
Artificial Disc Replacement: Replacing the damaged disc with an artificial one to maintain mobility. This option preserves more natural movement compared to fusion.
Discectomy: Removing the damaged portion of a disc to relieve nerve pressure. Often performed minimally invasively, leading to quicker recovery times.
Why Choose Us for Back Pain Treatment in Melbourne?
At Pain Specialists Australia, we combine cutting-edge treatments with compassionate care.
We’re proactive and get things done. We are back pain specialists in Melbourne and offer advanced care and treatment. We don’t give up.
Our experienced specialists create personalised treatment plans to target the cause of your pain, offering advanced interventions and holistic therapies to improve your quality of life.
Our aim is to get you on that planned holiday or social event, you are worried about missing out on.
Frequently Asked Questions (FAQ)
1. What exercises can relieve degenerative disc disease pain?
Gentle, low-impact exercises can ease pain and help your spine move better. Try walking, swimming, stretching, and core-strengthening exercises like pelvic tilts or bridges.
These movements reduce pressure on the discs, support your posture, and improve blood flow to your spine. Avoid twisting or heavy lifting unless guided by a physiotherapist.
2. What’s the best physical therapy for lumbar disc degeneration?
The best physical therapy targets strength, flexibility, and posture. A good program includes core exercises, gentle spinal mobility work, and stretches for the hips and legs.
A physiotherapist will tailor a plan to your pain level and movement goals. Hands-on therapy, education, and home exercises are often included for long-term success.
3. Can you prevent degenerative disc degeneration?
You can’t stop ageing, but you can slow disc wear with healthy habits. Stay active, keep a strong core, and use good posture when sitting, lifting, or moving.
Avoid smoking, manage your weight, and move often - even short walks help. These steps protect your spine and may delay or reduce the impact of disc degeneration.
4. Can degenerative disc disease be treated without surgery?
Yes, many people manage degenerative disc disease with non-surgical treatments. These include physical therapy, medications, lifestyle changes, and sometimes image-guided spinal injections.
The goal is to reduce pain, improve movement, and help you stay active in daily life. Physical therapy can strengthen your back and core, while medications ease inflammation and flare-ups. Changes like improving posture, staying mobile, and managing weight can also make a big difference over time. For many patients, these strategies work well and help avoid or delay surgery.
5. How long does it take to feel better with treatment?
Improvement varies from person to person, but many people start feeling better within a few weeks of beginning non-surgical care. This might include physical therapy, medications, or spinal injections.
Some treatments offer quick relief, like an injection that reduces nerve inflammation. Others take time, such as exercise programs that build strength and improve posture. For lasting results, consistency is key. Your recovery may also depend on how long you’ve had symptoms, your overall health, and how well you stick to the treatment plan.
6. How do I book an appointment with a back pain specialist in Melbourne?
Make sure you are not kept waiting for long periods of time before you get in to consult a Back Pain Specialist.
At Pain Specialists Australia, our experienced Pain Specialists will see 85% of referrals within the month of referral.
Contact Pain Specialists Australia today to schedule a consultation and start your journey to relief.
READY FOR RELIEF?
References
If you’re interested in more, here are some references for your perusal.
1. Cleveland Clinic – Degenerative Disc Disease Overview
- A trusted clinical resource explaining DDD, its symptoms, and conservative treatment options in simple terms.
https://my.clevelandclinic.org/health/diseases/16912-degenerative-disk-disease
2. Healthline – Degenerative Disc Disease: Symptoms, Causes, and Treatment
- Easy-to-read article that covers common questions patients have about DDD.
https://www.healthline.com/health/degenerative-disc-disease
3. Kapural L, et al. Radiofrequency intradiscal biacuplasty for treatment of discogenic lower back pain: A 12-month follow-up. Pain Med. 2015.
- This study supports the use of biacuplasty as a minimally invasive treatment for discogenic pain.
https://pubmed.ncbi.nlm.nih.gov/25339501/
4. Mohd Isa IL, Teoh SL, Mohd Nor NH, Mokhtar SA. Discogenic Low Back Pain: Anatomy, Pathophysiology and Treatments of Intervertebral Disc Degeneration. International Journal of Molecular Sciences. 2023; 24(1):208.
- In-depth open-access review of the biological changes in DDD and how imaging is used to assess it.
https://www.mdpi.com/1422-0067/24/1/208
5. Spine-health – Understanding Degenerative Disc Disease
- Comprehensive patient education article with diagrams that explain how and why discs degenerate.
https://www.spine-health.com/conditions/degenerative-disc-disease/what-degenerative-disc-disease
6. Non-Surgical Treatments for Degenerative Disc Disease: Can Injections Help?
- Our blog article on the various treatment options available
https://painspecialistsaustralia.com.au/blog/non-surgical-treatments-degenerative-disc-disease