Understanding Degenerative Disc Disease
Degenerative disc disease (DDD) is one of the most common causes of chronic back pain or sometimes referred to as discogenic back pain. It occurs when the intervertebral discs in your spine begin to change and break down over time. These discs act like cushions between your bones (vertebrae), allowing movement and absorbing the small day-to-day shocks to the spine.
As they change over time, they can become dehydrated and wear out, the space between the bones shrinks, the discs flatten, expand and bulge and become inflamed, which can irritate nearby nerves, restrict movement, and cause severe pain. For many people, this leads to ongoing stiffness, reduced flexibility, and discomfort during daily activities.
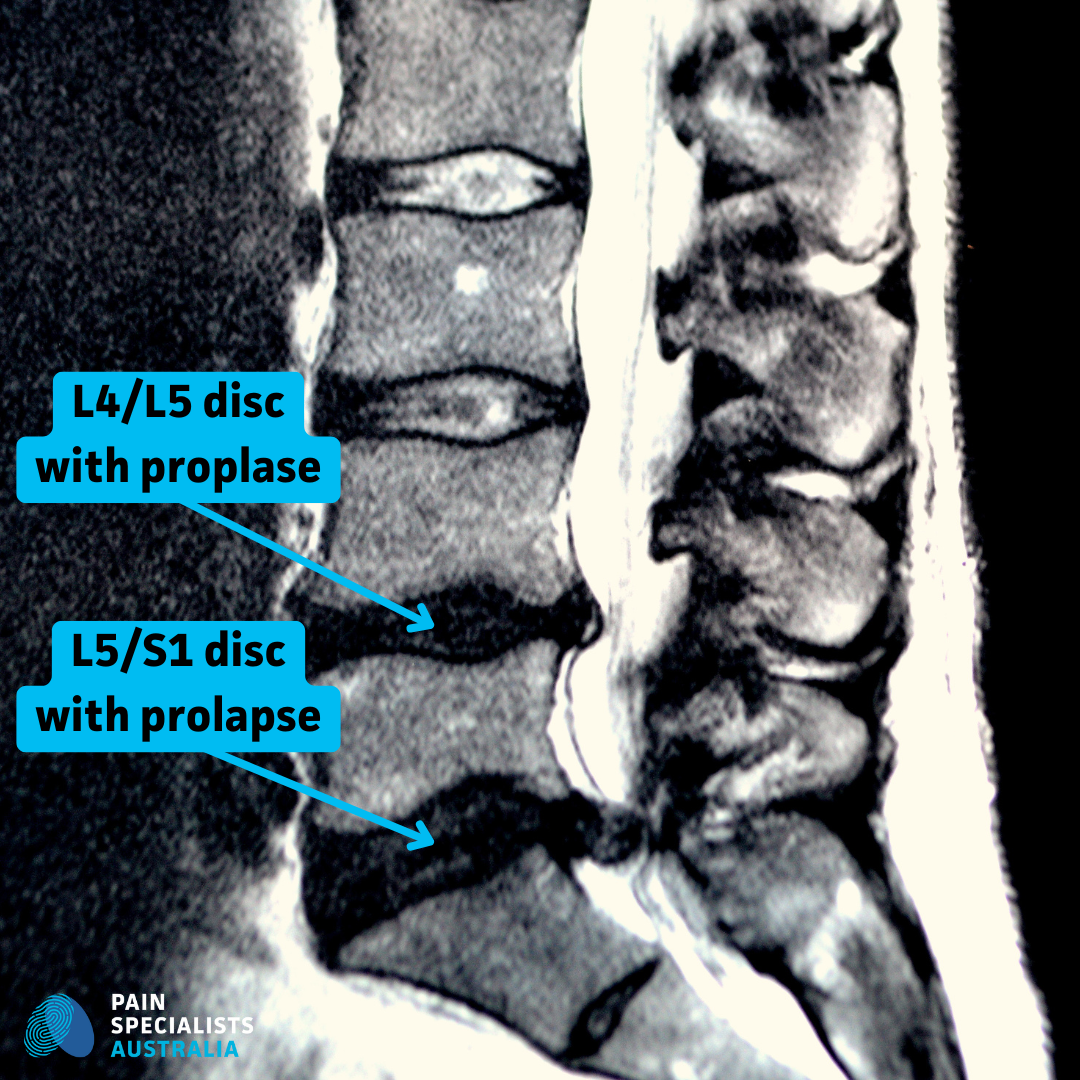
Degenerative Lower Lumbar Discs
Although DDD is linked to ageing, it can also result from repetitive strain, injury, or genetic factors. Importantly, not everyone with disc degeneration experiences pain, but when it becomes symptomatic, professional assessment and treatment are essential.
Common symptoms of degenerative disc disease include:
Chronic or recurring lower back pain.
Pain that worsens with bending, twisting, or sitting.
Numbness or tingling in the legs or buttocks.
Pain that improves with walking or lying down.
If you’re experiencing these symptoms, let’s assess it because early intervention can help you avoid more invasive treatments later.
Discover Your Back Pain Solution
Non-Surgical Treatment Options for Degenerative Disc Disease
At Pain Specialists Australia, we focus on non-surgical, image-guided treatments that help manage and reduce chronic back pain caused by DDD. Many of our patients come to us looking for alternatives to spinal surgery or medications that haven’t worked.
We develop personalised pain management plans that may include:
• Physical Therapy
Targeted movement and strengthening exercises improve posture and support the spine. A strong core and flexible back can significantly reduce disc-related pain and prevent flare-ups.
• Medications
Anti-inflammatory medications (NSAIDs), muscle relaxants, or short courses of nerve pain medications (anti-neuropathic agents) may be used to reduce inflammation and manage flare-ups.
• Lifestyle Modifications
Weight loss, posture changes, and ergonomic adjustments at home or work can relieve stress on your spine. Movement is often better than rest, especially with the right plan of action and support.
• Injection Therapies
For many people, image-guided spinal injections offer useful, targeted relief without surgery. These procedures are minimally invasive and can help you regain mobility.
Injection Therapies for Degenerative Disc Disease
Injection therapy is one of the most effective non-surgical options for managing pain associated with DDD. These treatments are performed by our experienced pain specialists using live imaging (such as fluoroscopy or ultrasound) to guide the needle precisely to the affected area.
The more common injections may include:
• Epidural Steroid Injections
Used to reduce inflammation around irritated spinal nerves, especially when disc degeneration leads to nerve root compression (such as sciatica). Pain relief may last from weeks to several months.
• Medial Branch Blocks and Nerve Blocks
These injections target the small nerves that send pain signals from the spine. If this work well, they may be followed by radiofrequency ablation for longer-term relief.
• Facet Joint Injections
When degeneration affects the small joints of the spine (facet joints), these injections can relieve localised back pain and improve mobility.
In some cases, patients may benefit from more targeted or advanced injection treatments which might include:
• Intradiscal Injections
These involve delivering heat or medication directly into the affected intervertebral disc.
• Intradiscal Biaculoplasty
Intradiscal biaculoplasty is a minimally invasive procedure that uses radiofrequency energy to reduce discogenic back pain by targeting the nerves inside a damaged spinal disc.
• Intradiscal Biologic Therapies (Emerging)
Includes platelet-rich plasma (PRP) and stem cell injections, aiming to promote disc healing or slow degeneration. These are currently under investigation and not yet widely adopted.
• Caudal Epidural Injections
This is a type of epidural injection delivered through the sacral hiatus at the base of the spine. It can be a good option for patients with multilevel degenerative changes or those who have difficulty tolerating traditional lumbar epidural injections.
• Sacroiliac Joint Injections
Although technically outside the lumbar spine, SI joint dysfunction often coexists with lower back pain from disc disease. To treat pain caused by compensatory joint strain or altered mechanics due to spinal degeneration.
• Trigger Point Injections
Muscle spasms and myofascial pain often accompany chronic back pain. Trigger point injections target tight muscle knots that may develop around the spine in response to chronic disc pain.
• Radiofrequency Ablation (RFA)
While not strictly an injection, RFA often follows diagnostic nerve blocks and can target painful spinal joints that may co-exist with degenerative disc disease. This can provide longer-term relief of facet-related pain or medial branch nerve pain, especially in patients with DDD-related facet arthropathy.
FAQs About Degenerative Disc Disease and Injection Therapy
Q1: What causes degenerative disc disease?
A: Degenerative disc disease happens when the spinal discs - which act like shock absorbers between your vertebrae - begin to wear out. This is often a natural part of ageing, but it can also be caused by repeated strain, spinal injuries, poor posture, or heavy physical work. Over time, the discs can dry out and lose their flexibility, which reduces their ability to cushion the spine. Genetics, smoking, and being overweight can also increase your risk of disc degeneration.
Q2: Are injection therapies safe?
A: Yes. When performed by trained pain specialists using live imaging such as ultrasound or fluoroscopy, spinal injections are considered low risk. These procedures are minimally invasive, should be performed in a controlled medical setting, and typically take only a short time to perform. Complications are rare, and most patients return to normal activities within a day or two. Your pain physician will always assess your medical history before recommending any procedure.
Your treatment plan depends on the cause of your pain, the location of disc degeneration, and how you’ve responded to other therapies. At Pain Specialists Australia, we use live imaging and detailed assessments to tailor your care.
Q3: How long does relief from injections last?
A: The duration of relief varies depending on the type of injection and the cause of your pain.
Some people feel better within a few days and can remain pain-free for several months.
Others may need repeated injections as part of a long-term treatment plan.
For some patients, injections provide enough pain relief to help them participate in physical therapy and return to normal activities without needing surgery or strong medications.
Q4: Can lifestyle changes help with DDD?
A: Absolutely. Staying active, losing excess weight, and improving your posture can make a big difference.
Regular low-impact exercise - like swimming, walking, or stretching - helps support the muscles around your spine and reduces pressure on your discs.
Quitting smoking and improving your workstation setup also support spinal health.
These changes don’t reverse disc degeneration, but they can reduce pain and slow the progression of the disease.
Q5: When should I consider injection therapy?
A: If your pain hasn’t improved after trying medications, physiotherapy, or other conservative treatments, your doctor may recommend an injection.
Injections are often used when disc-related inflammation is causing nerve pain or preventing movement.
They can be particularly helpful if your pain is limiting your ability to work, sleep, or stay active, or if you’re not ready or suitable for spinal surgery.
A pain specialist can assess whether you’re a good candidate based on your symptoms and imaging results.
Q6: Why Choose Injections Over Surgery?
Injections offer a safe and effective way to manage pain without the risks or recovery time of surgery. They can help you stay active, avoid opioid medications, and continue with physiotherapy or rehabilitation.
If you’re not ready for spinal surgery, or if surgery isn’t an option, injections may provide the pain relief you need to function better, sleep more comfortably, and return to normal activities.
READY FOR RELIEF?
References
1. Intradiscal Biacuplasty for Discogenic Low Back Pain: A Systematic Review
This review assesses the safety and effectiveness of intradiscal biacuplasty, a minimally invasive radiofrequency technique for treating discogenic pain.
Kapural L, Vrooman B, Sarwar S, Krizanac-Bengez L, Rauck R, Gilmore C, North J, Mekhail N. Radiofrequency intradiscal biacuplasty for treatment of discogenic lower back pain: a 12-month follow-up. Pain Med. 2015 Mar;16(3):425-31.
https://pubmed.ncbi.nlm.nih.gov/25339501/
2. Healthline - Degenerative Disc Disease: Can Injections Help Relieve Back Pain?
An accessible overview discussing how various injection therapies can alleviate chronic back pain associated with DDD.
3. Cleveland Clinic - Lumbar Epidural Steroid Injections: What It Is, Benefits, Risks & Side Effects
A comprehensive explanation of how lumbar epidural injections are used to manage back and leg pain caused by disc degeneration.
https://my.clevelandclinic.org/health/treatments/22091-lumbar-epidural-steroid-injection
4. Are Injectable Regenerative Therapies Effective in the Treatment of Degenerative Disc Disease? A Systematic Review
This systematic review summarizes current knowledge about injectable regenerative therapies, such as mesenchymal stem cells and platelet-rich plasma, in treating DDD.
DI Martino A, Barile F, Fiore M, Ruffilli A, Faldini C. Are injectable regenerative therapies effective in the treatment of degenerative disc disease? A systematic review. J Neurosurg Sci. 2022 Oct;66(5):399-405.
https://pubmed.ncbi.nlm.nih.gov/34342196/
5. Efficacy of DiscoGel in Treatment of Degenerative Disc Disease
A study evaluating the use of DiscoGel (percutaneous gelified ethanol) for managing discogenic pain in patients with lumbar DDD.
Latka K, Kozlowska K, Waligora M, Kolodziej W, Olbrycht T, Chowaniec J, Hendryk S, Latka M, Latka D. Efficacy of DiscoGel in Treatment of Degenerative Disc Disease: A Prospective 1-Year Observation of 67 Patients. Brain Sci. 2021 Oct 28;11(11):1434.
https://pubmed.ncbi.nlm.nih.gov/34827432/
6. Autologous Bone Marrow Concentrate Intradiscal Injection for the Treatment of Degenerative Disc Disease With Three-Year Follow-Up
An interesting study assessing the safety and feasibility of intradiscal bone marrow concentrate injections as an alternative to surgery for DDD.
Pettine KA, Suzuki RK, Sand TT, Murphy MB. Autologous bone marrow concentrate intradiscal injection for the treatment of degenerative disc disease with three-year follow-up. Int Orthop. 2017 Oct;41(10):2097-2103.