Chronic pain after surgery is different from normal healing pain and can persist for months or years after an operation.
Have you ever found yourself asking these questions?
“Why am I still in pain after surgery? I thought the surgery was supposed to stop it.”
“Why is my pain worse, or different, than it was before surgery?”
“If my surgery was successful, why do i still have pain?”
These are questions we hear often, and they point to a complicated issue: Persistent Post-Surgical Pain (PPSP), also known as Chronic Pain After Surgery. If you’re looking for a clear clinical overview of chronic pain after surgery, including how it is assessed and treated in a specialist pain clinic in Melbourne, see our Chronic Pain After Surgery webpage.
What is Persistent Post-Surgical Pain?
Chronic pain is now recognised as a disease in itself. Unlike acute pain from injuries, which fades as inflammation heals, chronic pain can persist even after healing. This type of pain isn’t unusual – it’s estimated that up to 1 in 5 people experience some form of PPSP. And while some surgeries are more likely to lead to persistent pain than others, any type of surgery, from minor dental work to major surgeries like knee replacements, has the potential to cause it.
Signs You May Have Persistent Post-Surgical Pain
PPSP typically shows up with certain signs:
Pain that starts or worsens after surgery.
Pain that lingers beyond the normal healing time, generally over 3 months.
Discomfort that can be felt at the surgery site or radiate to other areas nearby.
A sensation that resembles nerve pain, like tingling or burning.
The pain can feel unusually intense (hyperalgesia) or even occur with non-painful actions (allodynia).
If you’ve experienced these symptoms and your doctors have ruled out other causes like infection or cancer recurrence, PPSP may be the cause. This condition affects many patients, with studies showing that:
Up to 57% of patients experience PPSP after mastectomy.
Around 40% may have it following spinal surgery.
Knee replacements have an incidence rate of up to 44%, and hip replacements up to 27%.
Incidence of chronic postsurgical pain (CPSP), severe CPSP, and the proportion of neuropathic pain in CPSP [1]
Why Does Persistent Pain Happen After Surgery?
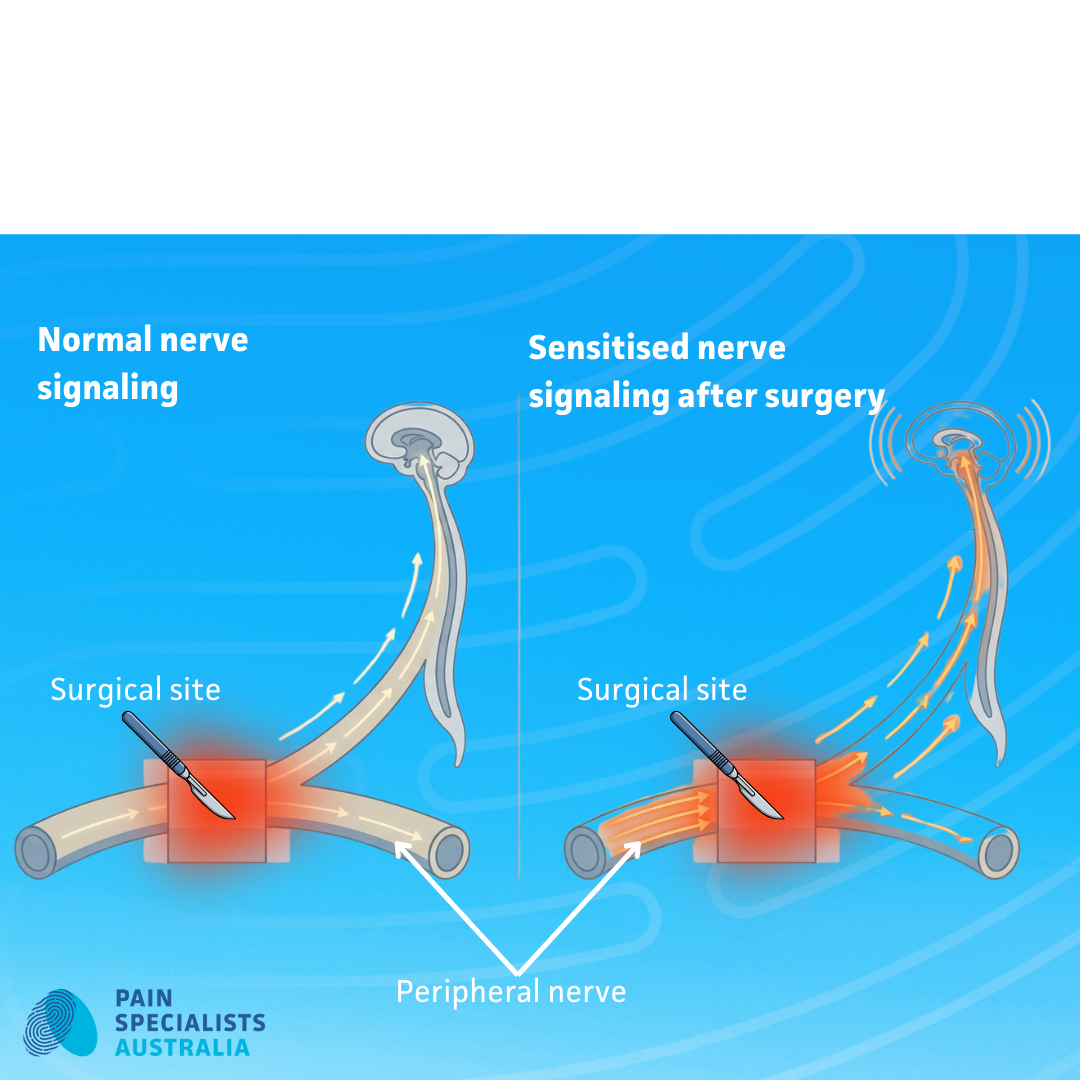
Surgery requires cutting through tissue and can lead to nerve damage. In some people, the tissue and nerves heal, but the pain lingers. Why? After an injury or surgery, our bodies release chemicals that activate certain nerve cells. This can lead to heightened nerve activity, changing the way our brains and spinal cords process pain. For some, these changes can make even small actions feel intensely painful.
Who’s at Higher Risk?
Certain factors can make PPSP more likely:
Poor pain control immediately after surgery.
Pre-existing chronic pain or post-operative complications.
Repeated surgeries in the same area.
Younger age, higher BMI, and emotional vulnerability are also factors.
Can Persistent Post-Surgical Pain Be Treated?
Treating PPSP requires a thoughtful, steady approach. Pain management specialists draw on a combination of therapies, including:
Medications to settle nerve pain.
Creams for skin sensitivity.
Nerve blocks and radiofrequency treatments to calm overactive nerves.
Advanced therapies like peripheral nerve stimulation and spinal cord stimulation.
Beyond these, education and physical and psychological therapies play a vital role. Patients learn strategies to manage pain and improve resilience, empowering them to improve their quality of life.
Prevention is Key
While PPSP can be treated, it’s easier to prevent than to reverse. If you’re planning for surgery, ask your doctor about ways to lower your risk of PPSP, such as discussing pain management strategies with your surgeon or anaesthetist.
Taking charge of your pain journey is about being proactive and open to exploring various strategies that could bring you lasting relief.
Ready to Take Control?
If you’ve been struggling with pain after surgery, don’t wait. Speak to a pain management specialist to explore treatment options and start taking steps toward relief today.
Chronic Pain After Surgery - Six Common Surgeries That Cause It, Prevention, Treatment
Pain Specialists Australia offers a variety of pain management treatment approaches for chronic pain.
Reach out today to discuss your options. Click the Contact Us button below to get in touch with our friendly team.
Schug SA, et al. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. PAIN. 2019;160(1):45-52.