Introduction
Almost everyone experiences back pain at some point in their life. It affects about 80% of adults, making it one of the most common causes of disability and sick days. Back pain can appear suddenly or develop gradually, affecting a small area or spreading widely across the back. While some cases are easily resolved, others can be persistent and difficult to treat.
Acute back pain lasts a few days to a few weeks and often resolves with self-care, leaving no long-term effects. Most acute back pain is mechanical, meaning there’s a temporary disturbance in how the spine, muscles, tendons, and ligaments work together. Think of the back as a complex machine: if one part malfunctions, the whole system can be affected.
Chronic back pain, on the other hand, persists for 12 weeks or longer, even after the original cause has been treated. It can be a significant challenge for both patients and healthcare providers.
What Makes Up the Lower Back?
The lower back is where most spinal pain occurs. It includes:
Five lumbar vertebrae (L1 to L5): These form the backbone of your lower spine.
Intervertebral discs: These act as shock absorbers, cushioning and supporting the spine during movement.
Muscles, ligaments, and tendons: These structures hold the spine together and allow movement.
Spinal nerves: 31 pairs of nerves extend from the spinal cord to control sensation, movement, and body functions. When compressed by a bulging disc, they can cause shooting pain down the leg, commonly known as sciatica.
Figure 1: Your lower back. (drawing by LadyofHats)
Figure 2: Some of the structures making up your lower back. (Drawing by Anuskafm under the GNU Free Documentation License.)
What Causes Lower Back Pain?
There are many potential causes of back pain, including:
Sprains and Strains: Overstretching ligaments or tearing muscles/tendons during improper twisting or lifting.
Spondylosis: Wear and tear on the spine as part of natural aging.
Facet Joint Syndrome: Osteoarthritis in the small joints between vertebrae, often treated with nerve blocks or radiofrequency neurotomy.
Sacroiliac Joint Syndrome: Arthritis or malfunction of the joints connecting the spine to the pelvis.
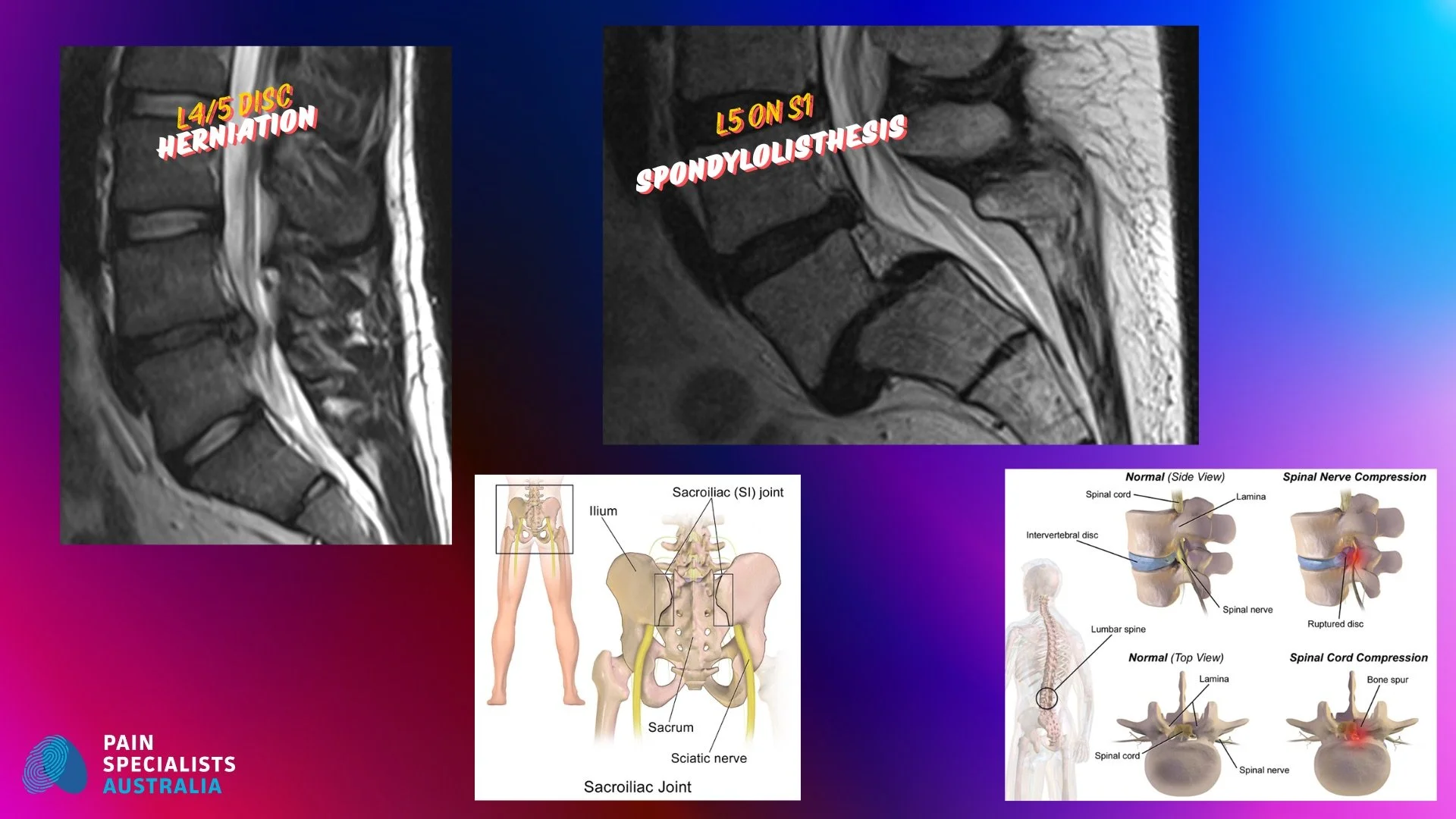
Figure 3: Sacroiliac joint and sciatic nerve. BruceBlaus. Under Creative Commons Attribution 3.0 Unported
Disc Degeneration: Loss of strength and elasticity in intervertebral discs, also called degenerative disc disease.
Herniated Discs: When discs bulge outward, compressing nerves and causing inflammation.
Spinal Stenosis: Narrowing of spaces in the spine, putting pressure on the spinal cord or nerves.
Figure 5: Spinal nerve compression (foraminal stenosis) or spinal cord compression (central canal stenosis) BruceBlaus Creative Commons Attribution-Share Alike 4.0 International
Sciatica: Irritation or compression of the sciatic nerve, leading to pain that radiates down the leg.
Spondylolisthesis: A vertebral bone slips out of alignment onto the bone below it.
Figure 6: Spondylolisthesis of L5 on S1 (PumpingRudi Creative Commons Attribution-Share Alike 3.0 Unported)
Trauma: Spinal injuries from accidents or falls.
Skeletal Abnormalities: Such as scoliosis, an abnormal curvature of the spine.
Red Flags: Serious conditions like fractures, infections, or cancers. Seek urgent medical help if you have severe, unrelenting pain, pain that worsens at night, or additional symptoms like unexplained weight loss, fever, or trouble moving your legs or controlling your bladder/bowels.
How is Lower Back Pain Diagnosed?
Diagnosing back pain typically involves a combination of:
Medical history and physical examination.
Imaging tests: X-rays, MRIs, or CT scans (only when necessary).
Special tests: Electrodiagnostics or blood tests in specific cases.
Risk Factors for Lower Back Pain
Some people are more prone to developing back pain due to:
Age: Aging leads to wear and tear, osteoporosis, and muscle stiffness.
Fitness Level: Weak back and abdominal muscles increase the risk.
Weight Gain: Extra weight stresses the spine.
Genetics: Conditions like ankylosing spondylitis have genetic links.
Occupation: Jobs involving heavy lifting, twisting, or prolonged sitting.
Pregnancy: Hormonal changes and weight redistribution often cause back pain, which usually resolves after delivery.
How is Back Pain Treated?
Simple Treatments:
Hot or cold packs: Reduce inflammation and ease discomfort.
Physical activity: Resume daily activities as soon as possible to improve flexibility and prevent complications.
Physical therapy: Strengthen core muscles and improve posture and mobility.
Yoga: Enhance strength and flexibility.
Medical Treatments:
Medications:
NSAIDs: Relieve pain and inflammation but carry risks like ulcers and cardiovascular issues.
Anticonvulsants: Calm overactive nerves (e.g., gabapentin, pregabalin).
Antidepressants: May help with chronic back pain.
Opioids: Reserved for short-term use due to risks of dependency and side effects.
Nerve Blocks: Diagnostic injections to pinpoint pain sources, often leading to radiofrequency neurotomy for long-lasting relief.
Radiofrequency Treatments: Heat applied to nerves to interrupt pain signals for months to years.
Epidural Steroid Injections: Temporary relief for inflammation-related pain.
Neurostimulation (Spinal Cord Stimulation): Implantable devices that modulate nerve signals to reduce pain.
Multifidus muscle restorative stimulation: is an advanced therapy designed to restore strength and function to the multifidus muscle, improving spinal stability and reducing chronic back pain.
Surgery: Reserved for severe cases like nerve damage or structural abnormalities. Options include spinal fusion, laminectomy, or artificial disc replacement.
Can Back Pain Be Prevented?
Many cases of back pain can be prevented by:
Maintaining a healthy weight.
Staying active with regular low-impact exercises.
Practising good posture.
Using ergonomic furniture and equipment.
Lifting objects correctly (from the knees, not the back).
Quitting smoking to improve spinal health.
Tips for a Healthy Back
Stretch before physical activity.
Use chairs with lumbar support.
Sleep on your side with knees drawn up or on a firm mattress.
Avoid prolonged sitting; switch positions and walk around regularly.
Invest in a height-adjustable desk for intermittent standing.
Conclusion
Back pain is a common but complex condition that can significantly impact daily life. Understanding its causes, prevention strategies, and treatment options can help you manage or even avoid it altogether. If your back pain persists, consult a medical professional or pain specialist for a personalised care plan.