Chronic Pain After Surgery
Chronic pain after surgery is real, common, and often misunderstood, especially when scans look normal, but pain persists or is worse than before the operation.
At Pain Specialists Australia in Melbourne, we assess and treat people with ongoing pain after surgery every day, focusing on clear diagnosis and mechanism‑based treatment.
Many people expect surgery to fix the problem. When pain continues months or years later, it can feel confusing, distressing, and isolating. You may be told healing is complete, yet the pain remains. For some, the pain is worse than before surgery or even has been caused by the surgery itself.
Our role is to explain why the pain persists, diagnose what is causing it and identify what is driving it. Once we have made a diagnosis, then we build a clear treatment plan to move forward.
Key takeaways
Ongoing pain after surgery is not rare and is often nerve-related.
This problem occurs in a significant minority of surgeries, particularly when nerves are involved.
Pain can persist even when healing looks complete on scans.
Surgery can trigger nerve injury or long-term pain sensitisation.
Early diagnosis improves outcomes and reduces unnecessary repeat surgery.
Specialist pain care focuses on diagnosing the cause, not just symptom control.
Why Am I Still in Pain After Surgery?
Many people ask this question when pain does not settle, as expected, months after an operation. We’ve explored this in detail in our blog, Why Am I Still in Pain After Surgery?, for those who want a deeper explanation. The short answer is that healing and pain are not the same thing.
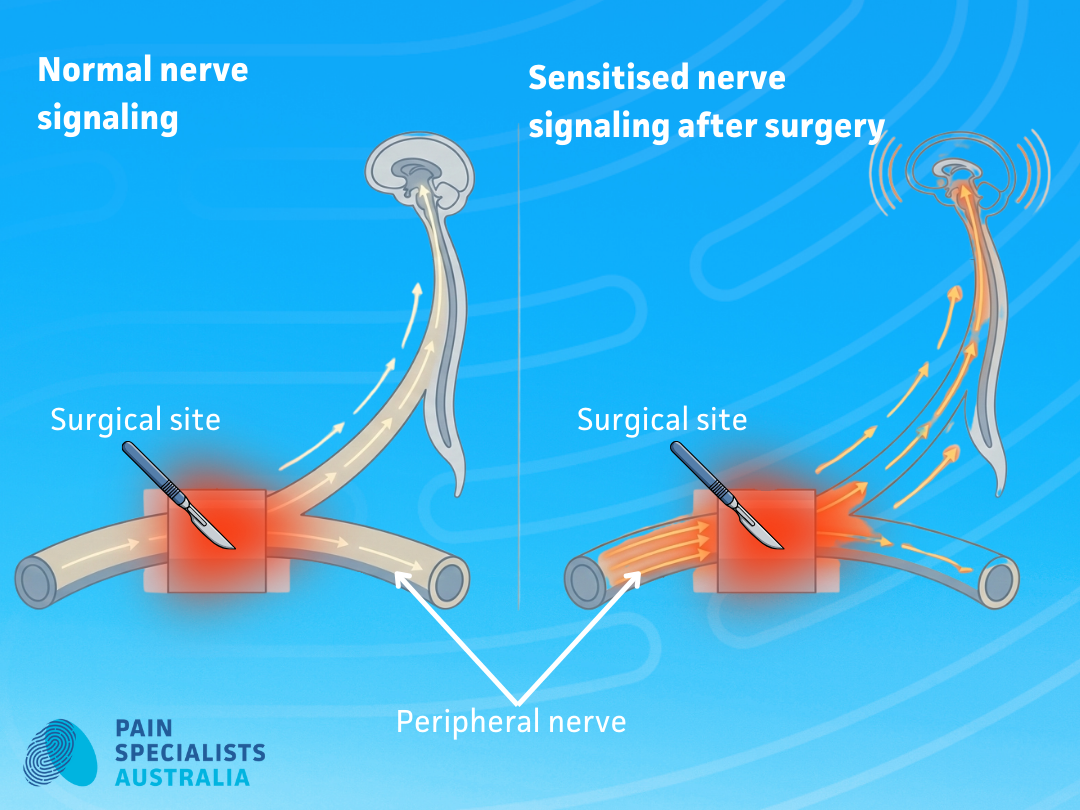
Surgery can change how nerves send pain signals, even after tissues heal.
Healing Has Finished, But Pain Pathways Have Changed
Tissues such as skin, muscle, and bone often heal within weeks or months. Pain, however, is produced by the nervous system. After surgery, nerves can remain irritated or overactive even when the surgical site looks healed. It is called nerve sensitisation.
Pain can continue without ongoing tissue damage.
Surgery Can Injure or Sensitise Nerves
During surgery, nerves may be:
Stretched
Compressed
Cut or scarred
Irritated by inflammation
Even minor nerve injury can lead to burning, stabbing, electric, or deep aching pain. In some people, the nervous system becomes more sensitive over time rather than settling. Night time pain is often nerve (neuropathic) pain.
Pain Can Become “Hard-Wired” Without Early Treatment
If ongoing pain and sensitisation is not recognised early, pain pathways can become reinforced. This process is known as pain sensitisation or nerve sensitisation or peripheral sensitisation or central sensitisation. The longer pain persists, the harder it can be to reverse without pain specialist input.
Is Ongoing Pain After Surgery Normal?
Some discomfort is expected after surgery. It should not be severe pain. Persistent pain that does not improve with tissue healing is different. It needs to be assessed early by pain specialists and treated early by experienced pain specialists.
When Pain Settles vs When Pain Persists
Pain is more likely to be part of normal recovery when it:
Improves steadily over time
Responds to simple measures
Matches the expected surgical recovery pattern
Pain is more concerning when it:
Persists beyond two to three months after the surgery
Worsens rather than improves
Feels tingly, burning, electric, or sharp
Is worse at night when you’re in bed
Limits sleep, mood, or daily function
Red Flags That Pain Is No Longer Part of Healing
Warning signs include:
Severe pain with normal imaging
Pain spreading beyond the surgical area
Sensitivity to light touch or clothing
Ongoing pain despite rest, medications and physiotherapy
These signs suggest nerve-related or sensitised pain rather than delayed healing.
Types of Surgery Commonly Linked to Chronic Post-Surgical Pain
Studies suggest that a significant number of people, often around one in five, develop longer‑term pain after surgery, with higher rates after spinal, knee, hernia, thoracic and breast procedures.
Some operations carry a higher risk of ongoing pain, especially when nerves are involved.
Chronic Pain After Spinal Surgery
Pain after spinal surgery may involve:
Nerve root irritation or injury
Scar tissue
Sensitised pain pathways
People may experience back pain, leg pain, burning, or numbness even when surgery is labelled a success.
The risk of ongoing pain varies by procedure.
Less invasive operations such as laminectomy or discectomy are generally associated with lower rates of persistent pain, particularly when nerve compression is clearly relieved.
More complex procedures such as spinal fusion carry a higher risk, as they alter spinal mechanics, place stress on adjacent segments, and may involve longer nerve exposure during surgery.
Across spinal procedures, many people continue to have ongoing or recurrent pain after surgery, especially when nerve‑related pain or long‑standing symptoms were present before the operation.
This does not mean surgery was the wrong choice. It does mean that persistent pain after spinal surgery often reflects how the nervous system has responded, rather than a simple structural problem that can be seen on imaging.
Chronic Pain After Joint Replacement (Knee, Hip, Shoulder, Foot)
Chronic pain after joint replacement is most common after knee surgery, though it can also occur after hip, shoulder, or foot procedures.
Pain may feel deep and aching, sharp with movement, or nerve-like with burning, tingling, or sensitivity around the joint. Some people continue to experience pain even when X-rays show good alignment and the joint moves well.
Knee replacements carry a higher risk of ongoing pain than hip replacements. The knee has a complex nerve supply, and nerves such as the saphenous nerve (which supplies sensation to the inner knee and leg) can be irritated or injured during total knee replacement. This may lead to persistent inner (medial) knee pain, sensitivity, or burning that does not improve with standard medications or rehabilitation. This is just an example of one of the many nerves around the knee that could be injured at knee replacement surgery.
Studies suggest that a notable proportion of people still have pain after knee replacement, even when the surgery is technically successful. In many cases, the pain reflects nerve irritation or sensitised pain pathways, rather than a problem with the implant itself.
Understanding the cause of pain after joint replacement is critical. Further surgery is not always helpful when pain is nerve-related, and targeted pain assessment can guide more effective treatment.
Chronic Pain After Hernia Surgery
Chronic pain after hernia surgery most often affects the groin or lower abdominal wall and may appear months or even years after the operation.
Pain is commonly sharp, burning, stabbing, or pulling, and may worsen with movement, coughing, or pressure. In many cases, nerves such as the ilioinguinal, iliohypogastric, or genitofemoral nerves can be irritated, scarred, or trapped during hernia repair, including mesh-based procedures.
A significant minority of people may experience ongoing pain after hernia surgery even when the hernia repair itself is intact. This pain is frequently nerve-related and does not show up on standard imaging.
When pain after hernia surgery is driven by nerve irritation or sensitisation, further surgery is not always helpful. A targeted pain assessment can help identify the source of pain and guide safer, more effective treatment.
Chronic Pain After Thoracic or Chest Surgery
Chronic pain after thoracic or chest surgery is well recognised and may persist long after the surgical wound has healed.
Procedures such as thoracotomy can irritate, stretch, or injure the intercostal nerves, which run between the ribs. This can lead to ongoing chest wall pain, burning, stabbing sensations, or marked sensitivity around the ribs and surgical scar. Pain may worsen with movement, deep breathing, coughing, or touch.
Many people develop ongoing pain after thoracotomy, often referred to as post‑thoracotomy pain syndrome. In many cases, pain is nerve-related and not explained by imaging or lung function tests.
When pain after chest surgery is driven by intercostal nerve irritation or sensitisation, repeated investigations or further surgery are rarely helpful. Targeted pain assessment can help identify nerve involvement and guide more effective treatment.
Chronic Pain After Pelvic Surgery
Chronic pain after pelvic surgery can be complex and may persist long after surgical healing is complete.
Procedures such as laparoscopy for endometriosis, hysterectomy, prostate surgery, or pelvic organ repair can affect intricate nerve networks within the pelvis. Nerves such as the pudendal nerve or branches of the pelvic plexus may be irritated or sensitised, leading to ongoing pain in the pelvis, groin, perineum, bladder, or bowel regions.
Pain may feel deep, aching, burning, or sharp, and is often worsened by sitting, movement, or bladder and bowel activity. Imaging is frequently normal, as nerve-related pelvic pain does not show structural damage.
When pelvic pain after surgery is nerve-driven or sensitised, further surgery is rarely helpful. A targeted pain assessment can help clarify the pain mechanism and guide safer, more effective treatment.
Chronic Pain After Abdominal Surgery
Chronic pain after abdominal surgery may persist long after the surgical site has healed and is often nerve-related.
Operations such as bowel surgery, gallbladder removal, or laparoscopic procedures can irritate or injure nerves within the abdominal wall. Nerves such as the anterior cutaneous branch nerves may become trapped or sensitised, leading to localised abdominal pain that is sharp, burning, or tender to touch.
Pain is often focal and may worsen with movement, muscle tension, or pressure. Routine scans are frequently normal because abdominal wall nerve pain does not cause visible structural changes.
When abdominal pain after surgery is driven by nerve irritation or entrapment, further surgery or repeated investigations are unlikely to help. A targeted pain assessment can identify the pain source and guide more effective treatment.
Chronic Pain After Breast Surgery
Chronic pain after breast surgery is well recognised and may persist long after surgical healing is complete.
Procedures such as mastectomy, lumpectomy, or breast reconstruction can irritate or injure nerves supplying the chest wall and upper arm. Nerves such as the intercostobrachial nerve or intercostal nerve branches may be affected, leading to ongoing pain in the chest, armpit, upper arm, or breast area.
Pain may feel burning, stabbing, tight, or sensitive to touch and clothing. Many people report pain despite normal imaging and reassurance that surgery was successful, as nerve-related breast pain is not visible on scans.
When pain after breast surgery is driven by nerve injury or sensitisation, further surgery is rarely helpful. A targeted pain assessment can help identify the pain mechanism and guide more effective treatment.
Why Scans Often Look Normal When Pain Is Severe
Normal imaging does not mean pain is imagined or minor. Imaging and scans only show structure; they do not show injured smaller nerves or nerve sensitivity.
MRI and CT Show Structure, Not Nerve Function
Scans detect infections, blood clots, fractures, tears, and alignment. They do not show nerve sensitivity or abnormal pain signalling.
Pain Is a Nervous System Output, Not a Damage Meter
Pain reflects how the nervous system processes signals. Severe pain can exist without visible tissue damage, especially after surgery. This is sometimes difficult to assess because the body and tissue is still recovering from surgery.
Why Chronic Pain After Surgery Is Often Missed or Poorly Managed
This type of pain often falls between specialties and can get misdiagnosed for year often leading to delayed treatment or worse outcomes.
Surgical Care Ends, But Pain Care Often Doesn’t Begin
Once healing is complete, patients may be discharged without a plan for persistent or chronic pain. Many are sent back to their GP without explanation or a treatment plan.
Many Doctors Are Not Trained in Post-Surgical Pain Syndromes
Chronic post-surgical pain is a pain specialist’s area of expertise. It requires training in nerve pain assessment, diagnosis, sensitisation, and multidisciplinary interventional pain management.
Many doctors and surgeons are not trained on the diagnosis and treatment of chronic pain after surgery, leaving far too many patients with unanswered questions and ongoing pain for years after their surgery.
Who Is More Likely to Develop Chronic Pain After Surgery?
Certain factors increase the risk of chronic pain after surgery, though risk does not mean that chronic pain is inevitable.
Factors Linked to Higher Risk of Ongoing Pain After Surgery
Chronic pain before surgery
Nerve-related pain before the operation
Previous surgery in the same area
High pain sensitivity
Undiagnosed or poorly managed anxiety or depression
Poor pain control early after surgery
Surgical complications or repeat surgery or long, complex surgery
Surgery Type Also Matters
Higher-risk procedures include the seven surgery types mentioned earlier:
Spine surgery – all forms of spine surgery and fusion surgery
Joint replacement, especially knee
Hernia repair
Thoracic surgery
Pelvic surgery
Abdominal surgery
Breast surgery
Risk Does Not Mean Inevitable
Understanding risk helps explain why pain persists and this guides better treatment. Early pain specialist assessment and diagnosis can reduce worsening pain and avoid unnecessary repeat surgery and save years of suffering without answers.
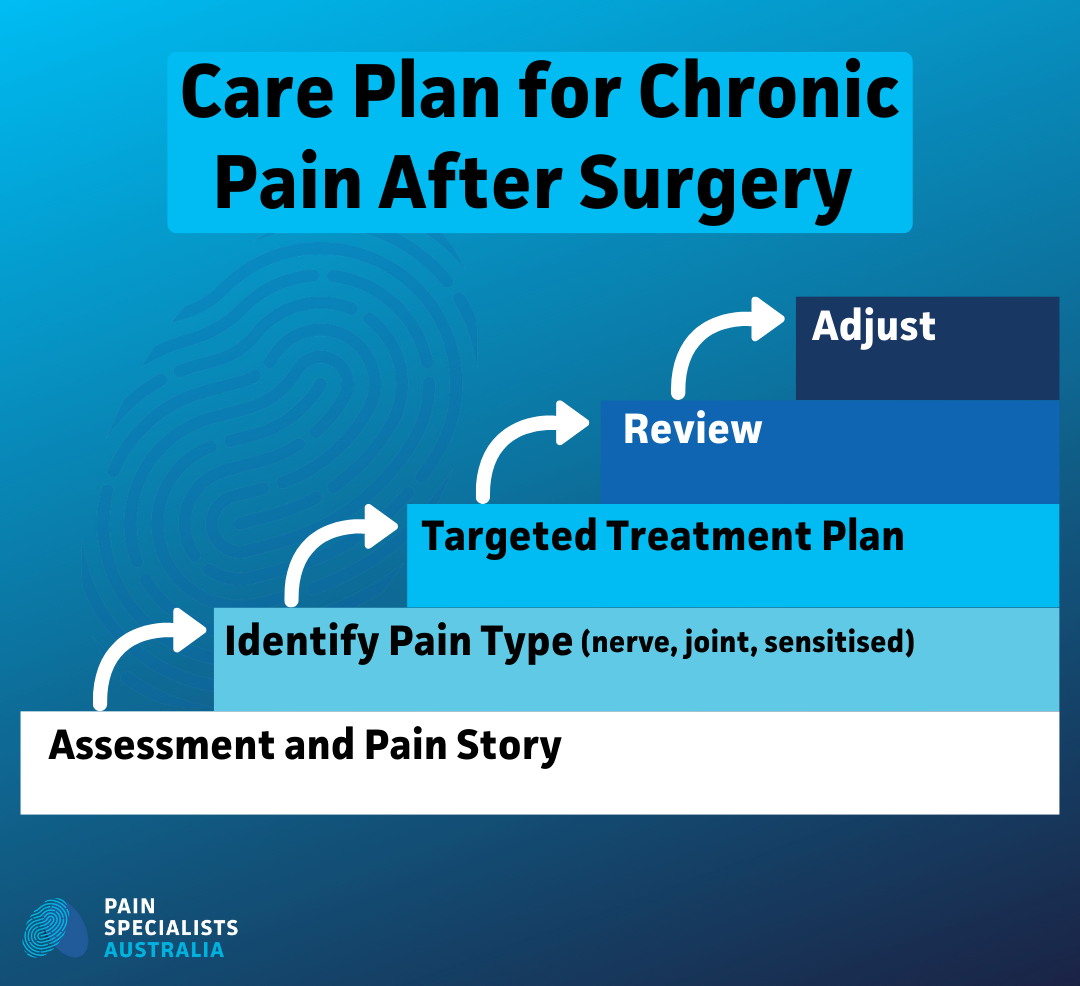
How We Diagnose Chronic Pain After Surgery
An early and accurate diagnosis is the foundation of effective pain treatment.
Listening to the Story of Your Pain
We start by understanding when pain began, how it feels, and what makes it worse or better. We must understand the pain and the context in great detail before we can diagnose it.
Identifying Nerve Injury vs Sensitisation vs Mechanical Pain
Pain after surgery is not always one condition. There can be many pain drivers and conditions for example the nerve pain may trigger a reduction in activity, which leads to weakness of muscles and stiffness of joints, which further worsens the pain. We assess whether pain is nerve-driven, sensitised, mechanical, or mixed.
Diagnostic Injections and Targeted Tests
Image-guided diagnostic procedures can help confirm pain sources and guide future treatment.
A structured, step‑by‑step approach helps identify the cause of ongoing pain after surgery and reduces unnecessary investigations.
A structured approach helps identify the cause of ongoing pain after surgery.
How Chronic Post-Surgical Pain Can Be Treated
There are multiple treatment options. The key is usually the right combination of different treatments all of which work on different systems/pathways. Treatment depends on the cause of the pain, the surgery, the patient and other factors not just the location of the pain.
Medication Review and De-Escalation
Many people remain on medications that no longer help esp. opioids. We focus on rational use of pain medications and reducing harm where possible. If it is nerve pain, then nerve medications can and should be considered.
Image-Guided Nerve and Pain Procedures
Targeted injections, nerve treatments, and radiofrequency techniques may reduce pain by addressing abnormal nerve signalling. For example a saphenous nerve block can be done to assess ongoing pain after a knee replacement.
Neuromodulation and Advanced Options
In selected cases, advanced pain treatments like neuromodulation can help regulate pain pathways when other treatments fail.
Rehab, Psychology, and Nervous System Retraining
Recovery often includes gentle guided movement, pacing, and strategies to calm an over-active nervous system. Using the right team to support these treatments is important.
Image-guided procedures can target nerve pain that persists after surgery.
Recovery often includes guided movement and nervous system retraining.
What People with Chronic Pain After Surgery Commonly Describe
We listen closely to what people share in clinics and online communities. These experiences shape how we care for every patient.
Common themes include:
“I was told the surgery was a success, but I’m worse.”
“No one can explain why I still hurt.”
“I feel dismissed because scans look normal.”
“I just want a plan that makes sense.”
These lived experiences highlight why early diagnosis and structured care matter. At Pain Specialists Australia, we work to replace confusion with clarity and fear with informed support. An early consultation, a formal pain diagnosis and a thorough treatment plan.
Why Choose Pain Specialists Australia?
People are often referred to us when pain persists, and answers are scarce.
All assessments are performed by experienced pain specialists.
Our doctors are fully trained in complex and interventional pain medicine.
We focus on diagnosis, not guesswork.
We offer advanced image-guided and neuromodulation treatments.
Care is coordinated with your GP, surgeon, and allied health team.
Once a referral is received, our team makes first contact with patients within 24 hours to arrange assessment at the most convenient Melbourne location.
Frequently Asked Questions (FAQ)
1. Why do I still have pain more than a year after surgery?
Pain can persist long after surgery even when healing is complete. This usually occurs when nerves are injured, irritated, or become over-sensitive during or after the operation. Scar tissue and changes in how the nervous system processes pain can also contribute. Scans may look normal because they show structure, not nerve function. A pain specialist focuses on identifying the pain mechanism rather than assuming surgery failed.
2. Is chronic pain after surgery common?
Yes. Ongoing pain after surgery is more common than most people realise, especially after spine surgery, knee replacement, hernia repair, and chest surgery. Many people are told pain will settle with time, but without early assessment, pain can become persistent. Recognising it early improves outcomes.
3. Can surgery cause permanent nerve pain?
Surgery can sometimes injure or sensitise nerves. That does not mean pain is permanent. Nerves can be treated and pain pathways can be modulated. The key is identifying the mechanism early rather than assuming nothing can be done once healing appears complete.
4. Why do scans look normal when my pain is severe?
MRI and CT scans show anatomy, not how pain signals behave. Chronic pain often reflects changes in nerve signalling rather than visible damage. This disconnect is frustrating for patients but well recognised in pain medicine. Diagnosis relies on clinical assessment, not imaging alone.
5. What treatments help when surgery didn’t fix the pain?
Treatment depends on the pain type. Options may include medication review, image-guided nerve procedures, neuromodulation, and coordinated rehabilitation. A tailored plan is more effective than escalating painkillers or repeating surgery without a clear diagnosis.
6. Who treats chronic pain after surgery in Melbourne?
Chronic post‑surgical pain is best assessed by pain specialists trained in nerve pain and complex pain syndromes. At Pain Specialists Australia in Melbourne, our team works alongside surgeons and GPs to diagnose causes and coordinate treatment, rather than focusing on one body part alone.
7. Should I have another surgery or see a pain specialist first?
If pain persists despite healing or worsens after surgery, seeing a pain specialist first is often helpful. A pain assessment can clarify whether further surgery is likely to help or whether pain is nerve-driven and better treated without more operations.
Start Your Assessment for Ongoing Pain After Surgery
Living with persistent pain after surgery can feel exhausting and uncertain. You do not have to navigate it alone.
Speak with your GP about a referral to Pain Specialists Australia. We focus on understanding the cause of your pain and building a plan that supports recovery and function.
References
Further Reading and References on Chronic Pain After Surgery:
1. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006 May 13;367(9522):1618–1625.
This landmark paper established chronic post-surgical pain as a distinct clinical condition rather than a complication of healing. It outlines nerve injury, sensitisation, and perioperative factors that increase long-term pain risk.
https://pubmed.ncbi.nlm.nih.gov/16698416/
2. Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Pain. 2009 Jul;144(3):253–255.
This paper explains how acute post-operative pain can transition into chronic pain through nerve injury and central sensitisation. It reinforces the importance of early identification and intervention to prevent long-term pain states.
https://pubmed.ncbi.nlm.nih.gov/19402781/
3. Werner MU, Kongsgaard UE. Defining persistent post-surgical pain: is an update required? Pain. 2014 Apr;155(4):736–737.
This article clarifies diagnostic criteria and reinforces that persistent post-surgical pain is not explained by ongoing tissue damage. It supports specialist assessment focused on pain mechanisms rather than imaging alone.
https://pubmed.ncbi.nlm.nih.gov/24554546/
4. Reddi D, Curran N. Chronic pain after surgery: pathophysiology, risk factors and prevention. Postgrad Med J. 2014 Apr;90(1062):222-7; quiz 226. doi: 10.1136/postgradmedj-2013-132215. Epub 2014 Feb 26. PMID: 24572639.
This review summarises biological and clinical drivers of chronic post-surgical pain, including nerve injury and altered pain processing. It highlights the importance of early, mechanism-based pain management strategies.
https://pubmed.ncbi.nlm.nih.gov/24572639/
5. Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Pain Med. 2010 Mar;11(3):332–341.
This guideline-based review supports targeted treatment of neuropathic pain rather than non-specific analgesic escalation. It provides evidence for mechanism-driven therapies relevant to post-surgical nerve pain.
https://pubmed.ncbi.nlm.nih.gov/20194146/
6. Deer TR, Mekhail N, Provenzano D, Pope J, Krames E, Leong M, et al. The appropriate use of neurostimulation: new guidelines and consensus statements. Neuromodulation. 2019 Feb;22(1):1–35.
This consensus document outlines evidence-based indications for neuromodulation in refractory chronic pain. It supports its role in carefully selected patients with persistent post-surgical and neuropathic pain.
https://pubmed.ncbi.nlm.nih.gov/25112889/
7. Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for ICD-11. Pain. 2019 Jan;160(1):19–27.
This IASP framework formally classifies chronic post-surgical pain as a recognised disease entity within ICD-11. It validates persistent pain as real, diagnosable, and deserving of specialist care.
https://pubmed.ncbi.nlm.nih.gov/30586067/
8. Christelis N, Simpson B, Russo M, Stanton-Hicks M, Barolat G, Thomson S, et al. Persistent Spinal Pain Syndrome: a proposal for Failed Back Surgery Syndrome and ICD-11. Pain Med. 2021 Apr;22(4):807–818.
This international consensus paper reframes “failed back surgery syndrome” as Persistent Spinal Pain Syndrome, shifting focus from surgical failure to pain mechanisms. It provides a modern, patient-centred framework that supports multidisciplinary and interventional pain management.