If your trigeminal neuralgia pain has returned after microvascular decompression (MVD), or relief didn’t last, you still have options. When repeat open surgery is not right for you, image-guided procedures can target the trigeminal system through tiny access points. This guide explains radiofrequency (RF), balloon compression, glycerol rhizotomy, and radiosurgery, plus when the sphenopalatine ganglion (SPG) treatment helps V2-dominant cheek pain, so you can plan next steps with your team in Melbourne, alongside your neurosurgeon and neurologist.
Why TN can return after MVD
Classical trigeminal neuralgia is often driven by an artery or vein contacting the nerve near the brainstem. MVD moves that vessel away or places a small pad on the nerve to protect it from the blood vessel. Pain can recur if contact persists or returns, scar tissue forms, or the original diagnosis evolves into a different facial pain pattern. A careful review helps decide whether repeat MVD or a percutaneous approach makes more sense.
Common triggers that can set off trigeminal neuralgia
Step 1: re-confirm the diagnosis
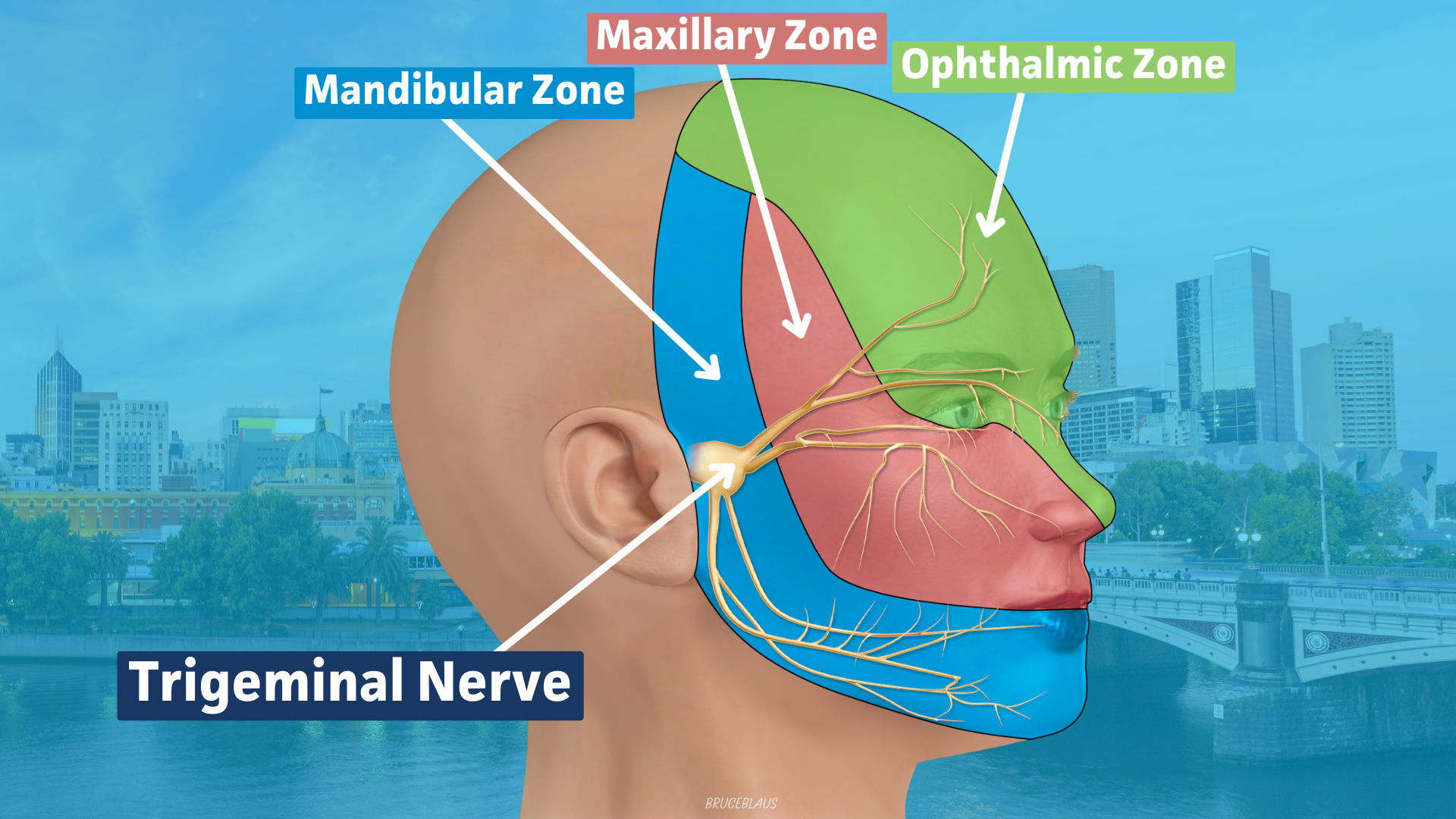
Focused clinical review of your pain pattern, brief electric-shock jolts, triggers and distribution.
MRI with a trigeminal protocol when appropriate, looking for ongoing neurovascular contact (also called conflict) or secondary causes (other possible causes of the pain).
Clarify whether this is still classical TN or shifting toward neuropathic facial pain, as this shapes procedure choice.
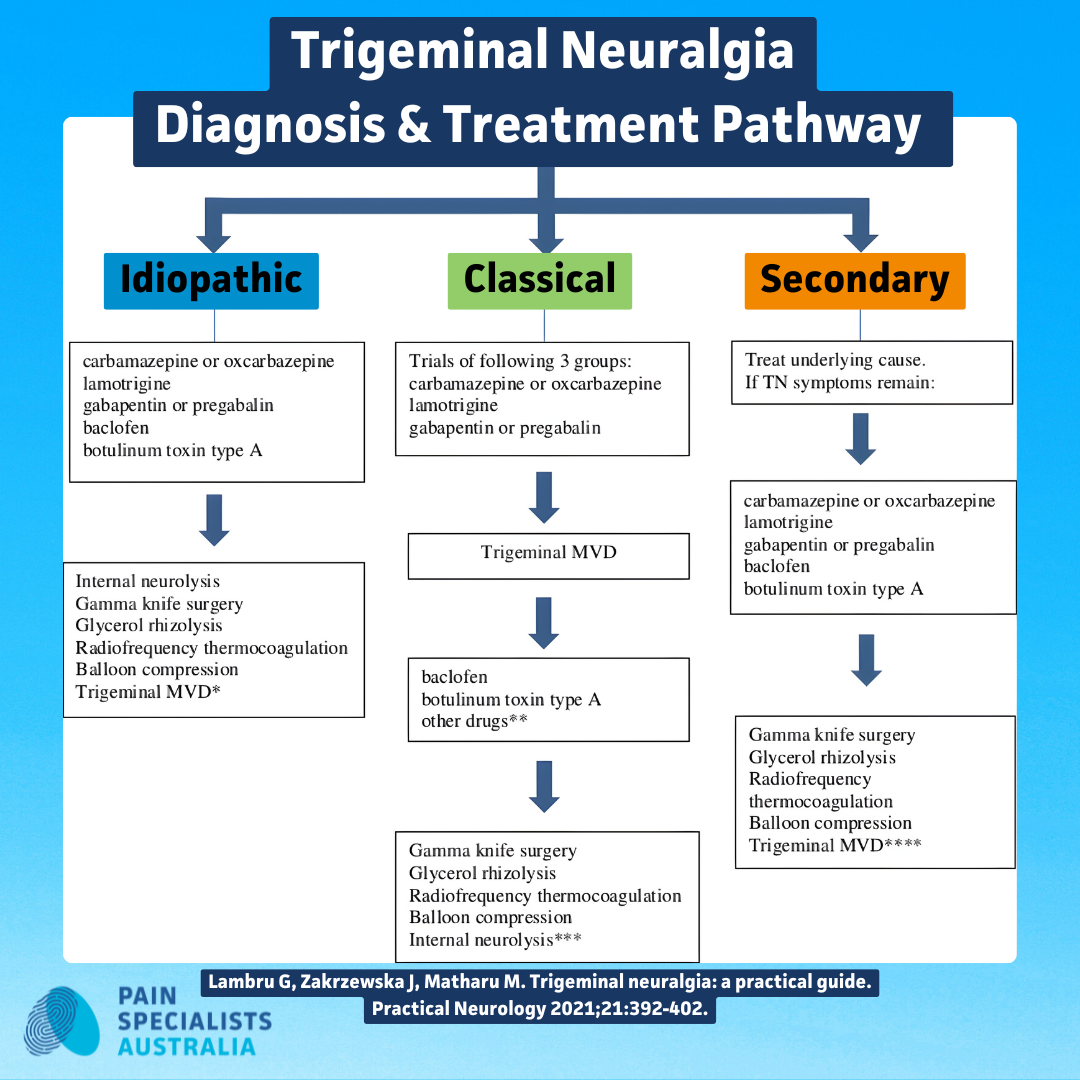
Your decision node: repeat MVD, percutaneous, or radiosurgery
Trigeminal Neuralgia Diagnosis & Treatment Pathway
Repeat MVD:
Consider if you are fit for surgery and imaging suggests persistent vascular contact. This will be discussed with your neurosurgeon.
Percutaneous procedures:
Done through the cheek with image guidance, under sedation. Recovery is generally fast recovery.
Radiosurgery:
Non-invasive outpatient option, relief develops over weeks to months. This is discussed and planned with your neurology team.
Radiofrequency for TN: how it works, what to expect
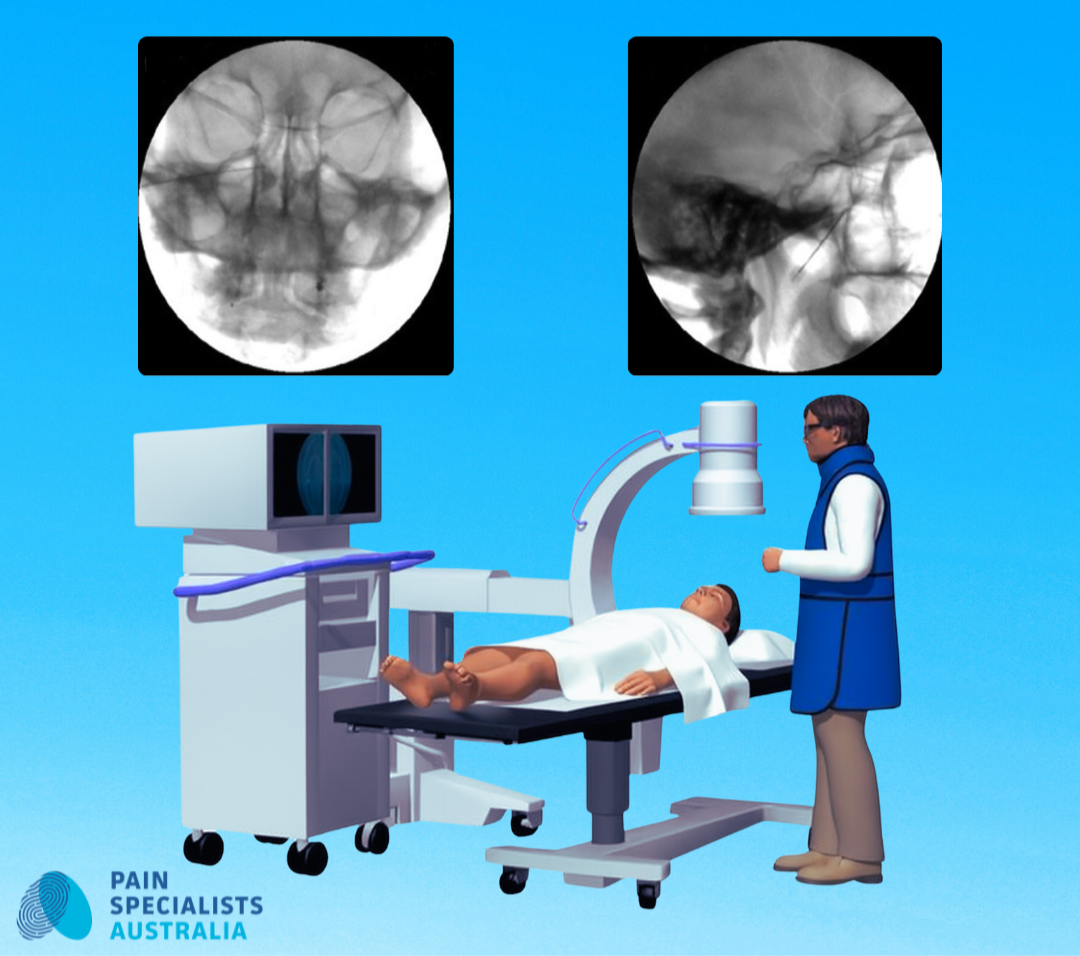
Image-guided trigeminal procedure in a fluoroscopy suite.
What it targets:
The Gasserian ganglion or specific trigeminal nerve divisions, with the aim of reducing abnormal or excessive pain signalling.
On the day:
Sedation, precise needle placement with X-ray guidance, test stimulation to confirm the right nerve (division), then a brief, temperature-controlled lesion, followed by an injection of local anaesthetic and steroid if appropriate.
Relief and durability:
Many people feel relief immediately or within a few weeks to six weeks; benefits can last months to years; procedures can be repeated if pain returns.
Sensation changes:
Some facial numbness or tingling can occur; we aim to minimise this and explain what to report after you go home.
Where RF fits:
A versatile choice after MVD when targeted lesioning is preferred, especially when V1 is spared or if the pain is predominately in V2 &/or V3 region.
Is RF right for you?
Balloon compression, glycerol neurolysis (rhizotomy), and radiosurgery: how they compare
Balloon compression:
Brief compression of the trigeminal ganglion with rapid onset; useful when multiple divisions are involved or when a very short procedure is preferred. Usually done by your neurosurgeon.
Glycerol rhizotomy:
A small amount of glycerol at the cistern selectively injures pain fibres; modest downtime. Usually done by your neurosurgeon.
Radiosurgery, for example Gamma Knife:
No incision; relief accumulates gradually; consider when invasive procedures are unsuitable or when a non-urgent option is acceptable. Usually done by your neurology team in conjunction with your neurosurgeon.
When SPG treatment helps, especially V2-dominant cheek pain
The sphenopalatine ganglion (SPG) sits behind the nose and links to maxillary pathways and autonomic features.
Who may benefit:
V2-predominant jolts, cheek or upper-jaw triggers, or mixed TN and neuropathic features.
What we offer:
SPG block as a diagnostic step or short-term aid, and SPG radiofrequency for longer relief in selected cases.
Expectations:
Relief can be time-limited and repeatable; we will map outcomes and decide when to repeat or switch modality.
Choosing the right percutaneous option: a practical matrix
Onset of relief:
RF and balloon are usually quick; glycerol is often also quick; radiosurgery is delayed.
Durability:
Varies by pattern and division; re-treatment is common and planned.
Sensory change risk:
Lowest aims with glycerol and radiosurgery; RF and balloon can produce targeted numbness, and we will counsel carefully.
Recovery time:
Percutaneous procedures are typically same-day; radiosurgery is same day with gradual effect.
Recovery, follow-up and what success looks like
We will track pain triggers with a simple diary, check sensation maps, and reduce medications if relief is stable. If pain recurs, we will discuss repeating the same procedure or changing modality based on how you responded the first time.
How PSA works with neurosurgeons
We review imaging together and coordinate care. Some patients are best served by a second-look MVD, and others by percutaneous or radiosurgical routes. Our role is to make that choice clear, safe and prompt. We work with your neurosurgeons and neurologists.
What people often say, common experiences
People commonly describe:
Lightning-like shocks when brushing teeth or a cool breeze on the cheek.
Relief after MVD, then jolts and pain sometimes return months or years later.
Worry about numbness, but have a preference for fast recovery and less disruption of life and daily activities.
We will discuss what each option means for triggers, sensation and downtime, in plain language.
Frequently Asked Questions
1. How long does radiofrequency relief last for TN
Relief often begins immediately and may last months to years. If pain returns, RF can be repeated or a different modality considered.
2. Is numbness after RF permanent?
Most sensory change is mild and settles over time. We aim for functional pain relief with the least sensation change possible and review you closely.
3. Does SPG treatment help cheek, V2, TN?
Yes, it can, particularly when V2 triggers dominate or there are autonomic features. We often start with a test injection or block to predict benefit before considering RF.
4. RF vs balloon compression, which is better?
It depends on your pain pattern and goals. RF allows very targeted lesioning; balloon can be preferable for multiple-division pain or if you want a very short procedure. We will explain trade-offs in sensation and durability.
5. When is repeat MVD worth considering?
If you are fit for surgery and imaging suggests persistent neurovascular contact, repeat MVD may be appropriate. If not, percutaneous or radiosurgical options provide strong alternatives.
References
Further Reading and References on Trigeminal Neuralgia and treatment:
1. Yan C, Zhang Q, Liu C, et al. Efficacy and safety of radiofrequency in the treatment of trigeminal neuralgia: a systematic review and meta-analysis. Acta Neurol Belg. 2022;122:1019-1030.
- Synthesises comparative cohort data including RF versus balloon compression, glycerol rhizotomy and MVD. RF provided high immediate pain relief with acceptable complication rates, positioning RF among first-line percutaneous options when medication or MVD are unsuitable.
https://pubmed.ncbi.nlm.nih.gov/33988820/
2. Asplund P, Blomstedt P, Bergenheim AT. Percutaneous balloon compression versus percutaneous retrogasserian glycerol rhizotomy for the primary treatment of trigeminal neuralgia. Neurosurgery. 2016;78(3):421-428.
- Retrospective cohort comparing balloon compression with glycerol rhizotomy as initial procedures. Both were effective, and the side effect profile favoured balloon compression with less dysaesthesia and corneal hypaesthesia.
https://pubmed.ncbi.nlm.nih.gov/26465639/
3. Parrent AG, et al. Percutaneous glycerol rhizotomy for trigeminal neuralgia in patients with multiple sclerosis versus idiopathic trigeminal neuralgia. J Neurosurg. 2019;132(5):1405-1413.
- Large single-centre series showing glycerol rhizotomy yields excellent acute pain relief in both MS-related and idiopathic TN. Durability is more limited and repeat glycerol rhizotomy remains effective when pain returns.
https://pubmed.ncbi.nlm.nih.gov/30978686/
4. Tuleasca C, Régis J, Sahgal A, et al. Stereotactic radiosurgery for trigeminal neuralgia: a systematic review and ISRS practice guideline. J Neurosurg. 2018;130(3):733-757.
- Systematic review and guideline supporting stereotactic radiosurgery as a non-invasive option with substantial rates of pain freedom. Onset is slower than with percutaneous lesioning, and sensory disturbance risk is linked to dose and targeting.
https://pubmed.ncbi.nlm.nih.gov/29701555/
5. Liu J, Wu G, Xiang H, et al. Long-term retrospective analysis of microvascular decompression in recurrent trigeminal neuralgia. Front Neurol. 2020;11:584224.
- Describes patterns of recurrence after MVD and outcomes with re-intervention. Carefully selected patients may benefit from re-exploration MVD or alternative interventions depending on imaging and intraoperative findings.
https://pubmed.ncbi.nlm.nih.gov/33408683/
6. Wu J, et al. Recurrence rates after microvascular decompression in primary trigeminal neuralgia and influencing factors: a systematic review and meta-analysis based on 8,172 patients. Front Neurol. 2021;12:738032.
- Noted a recurrence around 10% after MVD, with higher risk in atypical features, non-arterial compression and longer disease duration. These data help with counselling and with planning second-line options.
https://pubmed.ncbi.nlm.nih.gov/34659096/
7. Jiao L, Ye H, Lv J, Xie Y, Sun W, Ding G, Cui S. A Systematic Review of Repeat Microvascular Decompression for Recurrent or Persistent Trigeminal Neuralgia. World Neurosurg. 2022 Feb;158:226-233.
- Noted a recurrence around 13% after MVD. This paper summarises outcomes of repeat MVD, showing many patients achieve renewed pain control with acceptable complication rates when neurovascular conflict is identified. Supports re-exploration in selected cases after failed or relapsed MVD.
https://pubmed.ncbi.nlm.nih.gov/34875391/
8. Kanpolat Y, Savas A, Bekar A, Berk C. Percutaneous controlled radiofrequency trigeminal rhizotomy for idiopathic trigeminal neuralgia: 25-year experience with 1,600 patients. Neurosurgery. 2001;48(3):524-532.
- Seminal long-term series detailing technique and outcomes of RF thermocoagulation at the Gasserian ganglion. Demonstrates high immediate relief with defined sensory trade-offs that inform counselling.
https://pubmed.ncbi.nlm.nih.gov/11270542/
9. Jia Y, Pan Y, Ren H, Ji N, Luo F. Effectiveness and Safety of High-Voltage Pulsed Radiofrequency to Treat Patients with Primary Trigeminal Neuralgia: A Multicenter, Randomized, Double-Blind, Controlled Study Protocol. Pain Physician. 2018 Sep;21(5):469-481.
- A major clinical trial is testing whether high-voltage pulsed radiofrequency — a precise, non-destructive nerve treatment — can provide longer-lasting pain relief than standard nerve blocks for people with trigeminal neuralgia whose pain no longer responds to medication.
Early results showed that high-voltage pulsed radiofrequency provided better and longer-lasting pain relief than nerve blocks, with many patients reporting significant improvement and few side effects.