Choosing a Pain Clinic in Melbourne: What Actually Matters
Choosing the right pain clinic is one of the most important decisions you can make when pain does not improve.
People can tolerate pain longer than they should, but what often breaks them is not being believed, being rushed, or being told to “try this and come back later” without a clear diagnosis or plan.
If you are comparing pain clinics in Melbourne, two questions, that patients ask, matter more than any other:
Will I get a proper diagnosis and a clear treatment plan delivered by an experienced and committed pain specialist?
Will I be left waiting without direction?
Pain Specialists Australia (PSA) is a well-established, high-functioning pain clinic.
Referrals are contacted within 24 hours of receipt, care is proactive, and assessment focuses on a working diagnosis and a treatment plan discussed from the first consultation.
Our team includes experienced, full-time pain specialists who use the full breadth of treatment options, from lifestyle strategies to advanced pain procedures.
We are supported by on-site administrative staff who guide patients through every step of care.
Assessment focuses on diagnosis and direction from the first consultation, not trial-and-error.
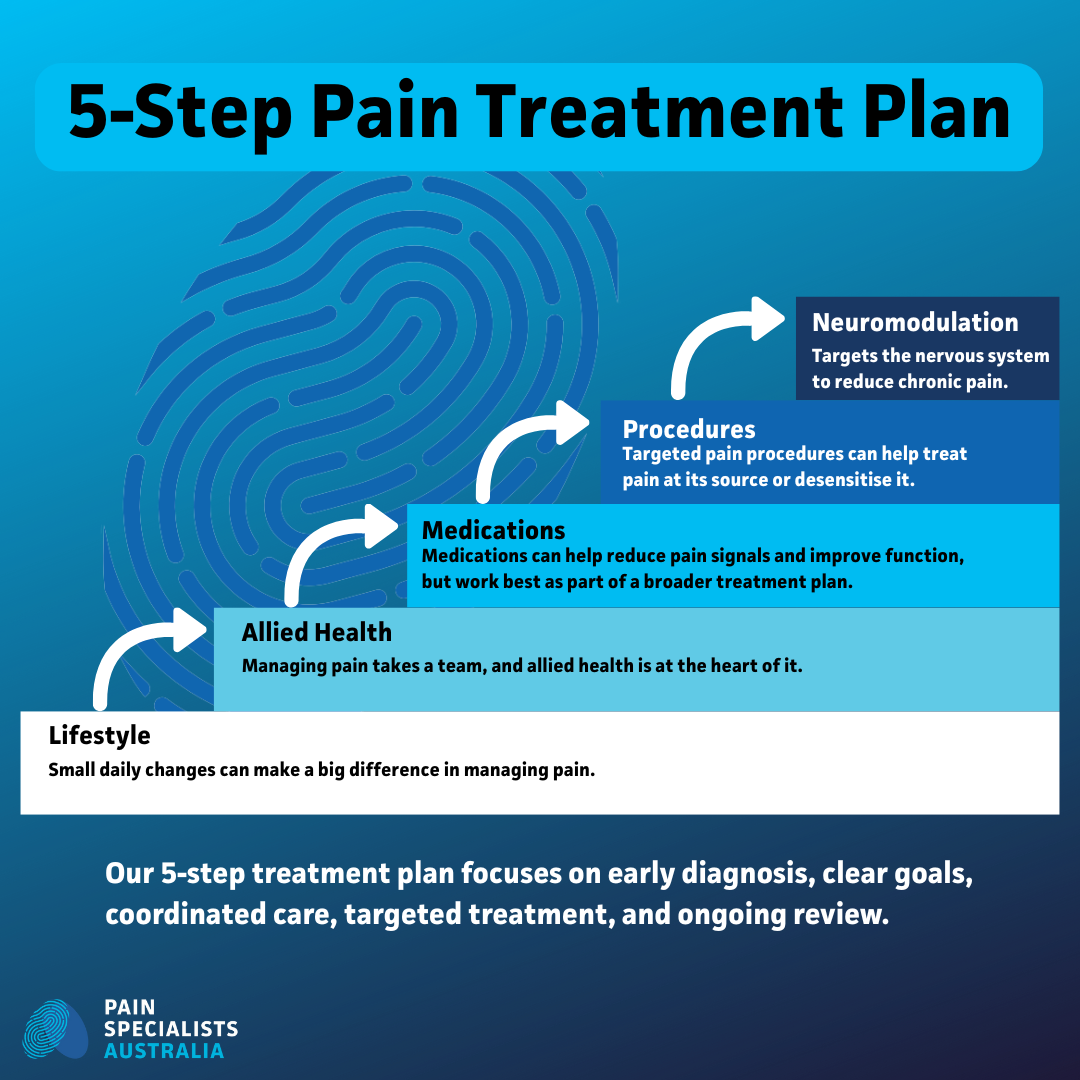
PSA’s 5-step pain treatment plan focuses on diagnosis first, coordinated team care, targeted treatments, and ongoing review.
Key takeaways
Speed matters.
Long waits for consultations delay care. They can allow pain to settle in and become harder to treat. Some private clinics have long-wait time for consultations. We don’t. Many public pain services also run long waiting lists. We don’t.
Admin care matters.
Real people who answer the phone, listen, follow things up, and guide you through the system make a major difference when you are already overwhelmed by pain.
Breadth matters.
Pain is not one-dimensional. Hence, you need access to multiple treatment options, not a single treatment approach applied to everyone.
Teamwork matters.
When clinicians work in silos, patients receive mixed messages and are more likely to fall through the cracks. A coordinated team reduces confusion and wasted time.
Every patient receives a clear pain diagnosis and personalised treatment plan from day one at Pain Specialists Australia.
Pain Specialists Australia vs “typical” pain clinic models
Service models in pain care vary widely. Below are common patterns reported across private and public pain services compared with PSA’s stated model of care.
Patients contacted within 24 hours of receipt of referral.
Diagnosis and treatment plan from first consult.
Urgent cases like CRPS and other nerve pains triaged.
MDT (Multidisciplinary Team) review for complex cases.
Full-time pain specialists.
Clinics vary. The table below compares common patterns across private and public pain services with PSA’s stated model of care and service standards.
How to choose a pain clinic
Ask these 9 questions when choosing a pain clinic:
How fast will you contact me after my GP sends a referral?
How long before my first appointment?
Does the clinic have a full complement of full-time admin staff on site?
Who helps me get tests, reports, and bookings sorted?
Will I get a clear diagnosis and a treatment plan of action at first consult?
Do clinicians work as a team, or as individuals?
What happens if pain flares or care stalls?
What options exist beyond medication?
Can urgent cases be prioritised?
Frequently Asked Questions
1. What is the best pain clinic in Melbourne?
Best means “best fit”. Look for fast access, expertise, teamwork, getting a clear diagnosis and a treatment plan of action, coordinated care, and options beyond one approach. A clinic that contacts referrals quickly and gives a plan early reduces months of drift.
2. How long is the wait for a public pain clinic in Australia?
Wait times vary by hospital and triage category. National reviews of Australian persistent pain services have reported capacity and access pressures, with waiting being a recurring system problem.
3. How do I get seen faster for suspected CRPS or other acute serious pain conditions like neuropathic (nerve) pain?
Ask your GP to flag your possible pain diagnosis clearly on the referral and include onset date, limb changes, and functional impact. Ask the clinic about urgent triage pathways. Early review matters because delay can entrench disability.
PSA uses experienced clinical nurses to triage referrals, with direct support from pain specialists where required.
4. Do I need scans before seeing a pain specialist?
Often, no. Scans can help, but pain diagnosis is not scan-only. A proper assessment uses history, exam, prior responses, and targeted testing where useful.
5. Should a pain specialist give a diagnosis at the first visit?
A responsible pain specialist should provide a working diagnosis and full plan at the first consultation, even if further information is needed. Leaving patients without direction prolongs suffering.
6. What does “multidisciplinary pain care” mean?
More than one discipline working on one plan. Many public clinics use interdisciplinary models. In private care, quality depends on whether the team is integrated or siloed.
7. Are multidisciplinary teams important?
Yes, especially for complex pain. MDT discussion improves decision-making and reduces siloed care.
8. Are all pain clinics the same?
No. Training, scope, team structure, admin support, and speed vary widely. Use the checklist above.
9. Why does feeling dismissed matter in pain care?
Feeling dismissed worsens outcomes. It increases stress, reduces trust, and can amplify pain itself. Good pain care starts with being heard and never dismissed.
References
1. Hogg MN, Kavanagh A, Farrell MJ, Burke ALJ. Waiting in Pain II: An Updated Review of the Provision of Persistent Pain Services in Australia. Pain Med. 2021;22(6):1367–1375.
- National Australian review showing persistent pain services face ongoing access and capacity pressures, with long waiting times remaining a major barrier to timely diagnosis and treatment. Strongly supports the importance of early access and proactive care models.
https://pubmed.ncbi.nlm.nih.gov/33106875/
2. Hogg MN, Gibson S, Helou A, DeGabriele J, Farrell MJ. Waiting in pain: a systematic investigation into the provision of persistent pain services in Australia. Med J Aust. 2012;196(6):386–390.
- Landmark Australian study documenting significant gaps in access, staffing, and service provision across public pain clinics. Frequently cited in national policy discussions and underpins why delays in pain care remain a systemic issue.
https://pubmed.ncbi.nlm.nih.gov/22471539/
3. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;350:h444.
- High-level evidence demonstrating that multidisciplinary, team-based pain care leads to better long-term pain and functional outcomes compared with usual or fragmented care. Supports the importance of coordinated MDT models over siloed treatment.
https://pubmed.ncbi.nlm.nih.gov/25694111/
4. Harden RN, Bruehl S, Perez RSGM, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain. 2010;150(2):268–274.
- Key validation study confirming that the Budapest Criteria improve diagnostic accuracy for CRPS compared with older criteria. Reinforces the need for early, diagnosis-led assessment and urgent triage pathways for suspected CRPS.